The first time seeing the northern lights in my backyard on 3/23/23. Stunning.

Let me make something clear from the start: Sandra Allen’s A Kind of Mirraculus Paradise: A True Story About Schizophrenia really is a piece of anti-psychiatry propaganda.
The book opens with the author recalling how their estranged uncle, “crazy” Bob, had contacted them shortly after Allen had enrolled a graduate writing program. Upon learning that Allen is a writer, Bob calls them to say, “Hey, I wrote a book, man. I wrote the story of my life.” Not too long after that, Allen receives a bizarre manuscript from Bob in the mail, along with a note apologizing for its “messiness” and an offer to pay for Allen’s services. Of Bob’s typewritten transcript, Allen writes that it was “hideous to look at, even from a distance,” describing a “wall of text” in “almost exclusively capital letters, with no paragraph breaks” and “colons everywhere.” Allen thought it “stank like cigarettes.” Upon reading through several pages, Allen considered the possibility that Bob’s story might be a product of delusion or a calculated lie. Allen continued to read Bob’s manuscript, but when some of the language became “explicitly racist,” Allen chose to disengage. As Allen tells it: “I wanted to ignore it the way you ignore a urine-soaked pile of coats on a sidewalk or a man on a park bench screaming obscenities.”
AKOMP is not about schizophrenia, but about feeling toward schizophrenia. It’s is an experimental and contentious narrative, elegant in its execution and almost deficient in every other way. The author, Allen, an accomplished journalist and editor, takes on the topic of schizophrenia from an unconventional and experimental angle. The book oscillates between these two different narratives written in different fonts. In the first narrative, Allen tells Bob’s story. In the second narrative, Allen attempts to address larger issues pertaining to mental illness by investigating the conceptual and diagnostic meaning of schizophrenia, as well as the changing ways American psychiatry has treated madness. “I am no expert in so many of the complicated topics at hand,” Allen concedes early in the book. While Allen promises to vows to “compensate” by learning as much as possible, it quickly becomes painfully apparent that Allen hasn’t put in the research.
Allen’s own “reportage” on mental illness is dismal, unrigorous and tinged with a distinct moralizing anti-psychiatry ethos that bodes ill for the rest of the project. The book contains significant errors. The author’s reliance on several single-minded, simplistic talking-points mar what is otherwise an eloquent and entertaining experimental illness autobiography.
The first page of Bob’s manuscript, his own writing (in lowercase): “this is a true story of a boy brought up in berkeley california durring the sixties and seventies who was unable to identify with reality and there for labeled as a psychotic paranoid schizophrenic for the rest of his life.”
This theme of truth and veracity is invoked and reinvoked throughout the book. Allen recounts, somewhat regrettably, conducting a meticulous, fact-checking of her uncle’s story, including interviewing family and “comparing Bob’s facts with what I could confirm elsewhere in letters, report cards, resumes, and the accounts that people were giving me.” Allen’s investigation of the world around Bob strikes at the core theme of the book.
Allen seems to fear the delusion of Bob’s account of reality. And yet, Bob’s narrative is not where the careful reader should cast their suspicions. It’s Allen’s so-called “journalism” that has more in common with a Washington Post op-ed or Mad In America blog or Tom Friedman column than anything that is verifiable, fact-checked, and deeply committed to accuracy.
There are errors in AKOMP and they are chiefly mischaracterizations of medical treatment. Case in point, in a passage occurring about halfway through the book, Allen claims that psychiatric medications such as antidepressants and antipsychotics medication are “addictive” because “some” patients who “choose” to stop taking them often experience withdrawal symptoms.
Some people who’ve chosen to quit neuroleptics often find that comes with an excruciating period of withdrawal. Some feel that the addictiveness of these drugs isn’t sufficiently studied or communicated to patients.
In the passage above, Allen hopes you will conflate drug dependence and drug withdrawal with drug addiction and accept this unsubstantiated claim, which is a prominent talking point in anti-psychiatric circles, then assume that withdrawal from prescribed neuroleptic medication is just as harmful as someone withdrawing from heroin or opioids.
But let’s read this more closely and think about what is going on here. Allen is trying to convince us that prescribed neuroleptic withdrawal constitutes an “addiction” for those who choose to stop taking these drugs. Yet, drug dependency and withdrawal occur with many prescribed and legal nonprescription substances, sometimes resulting in “an excruciating period of withdrawal” for “some people.” Furthermore, if we understand the concept of addiction to involve some element of pleasure or positive reinforcement that leads a person to misuse or abuse a substance, it becomes even less compelling to argue that antidepressants or antipsychotic drugs are “addictive.” That’s not to discount the seriousness of withdrawal, which can certainly be “excruciating,” but they hardly fulfill addiction criteria. If I were to guess, however, I’d say that Allen is trying to push an anti-medication agenda, while appearing to offer a “critical” and “balanced” account of a complex topic. With the neat phrase “some people,” these words are divorced from their author and neutralized of their intent. It’s an incredibly irresponsible approach that Allen adopts throughout the project.
In another example, Allen unsubstantiated claim that “electroshock therapy” can cause comas should stick out like a thousand sore thumbs.
[Agnes] recalled hearing he had undergone electroshock therapy at Herrick Hospital. Gene wasn’t sure whether that was the case; Bob made no mention of it in his manuscript. (The controversial therapy can cause memory loss and comas.)
The parenthetical is key. A citation or example would go along way here. But Allen provides no evidence whatsoever, even anecdotally, that comas are a side effect of ECT. Probably because there isn’t any. While a cursory Google search on the topic came up empty, a colleague managed to find a single article from the Journal of Clinical Psychiatry reporting a case of coma occurring in a psychotically depressed man. But it wasn’t the ECT. Rather, the source of coma was reportedly due to the IV administration of droperidol during post-operative recovery. This article contains 9 citations and none of them lead to another relevant case.
It would be one thing if these two instances of unsupported and questionable examples of bullshit claims masquerading as facts were honest mistakes in an otherwise “true account of schizophrenia.” But, of course, they’re not. Other mistakes fall into two overlapping categories: poorly researching the issues and rhetorical strategies.
As Allen explained in one interview, an additional goal of this book is to successfully address bigger questions concerning mental illness, such as: “What is schizophrenia, what is mental illness? What is known about a category like schizophrenia and what is not known?” Compounding my discomfort with this book is the author’s superficial treatment of this topic.
Repeatedly, Allen writes of “some people” as if they are a meaningful metric. “Some people.” Who are they? No one knows. How many of them are there? Some. How many is “some”? 5? 20? 100? No one knows.
Some people feel that no amount of research will ever yield answers to basic questions about schizophrenia because the word ‘schizophrenia’ doesn’t refer to any actual disease. They argue that psychiatric diagnoses only reflect the biases of those giving them, whether individual or social. They point to antique diagnoses that, in hindsight, betray this phenomenon completely.
Certainly, the existence of multifarious reactions to the etiology of schizophrenia, the validity of the diagnosis itself, and the potential for research to find answers need no citation, but by offering zero studies, data, examples or empirical basis for such a claim, Allen’s statement is useless. Why is Allen writing any of this? What is the point? What exactly are we talking about here?
In my experience, people who’ve been psychiatrically diagnosed feel a variety of ways about their diagnosis and about the field of psychiatry itself. Some who’ve been told they have schizophrenia agree with the diagnoses, and some feel that psychiatric medication has saved their lives. Others of the opposite persuasion champion for the abolition of psychiatry entirely.
Allen engages in a false dichotomy, presenting the experience of diagnosis and of the psychiatric discipline as either cheerleaders of the life-saving benefits of psychiatry and, notably, psychotropic medication, or the opposing “critical” anti-psychiatry anarchists, who’ve read the writing on the wall, and seek to burn the psychiatric establishment to the ground. It’s an argument that don’t really need to “proven” or justified with evidence since it’s nearly impossible to argue with.
No two people I’ve interviewed or resources I’ve read about mental health care in America have felt the same way about what the right treatment should look like. But most everyone who follows these issues agree that the situation at present is quite grim.
You certainly don’t have to cite your own experience, but statements as abstract as this require context and elaboration. It should be easy to name one person among series of “no two people” and “most everyone.”
As some alternatives have taken root in this country in recent decades, others have worked to oppose them.
That’s great. But what alternatives are you talking about? Rhetorically, these “both sides” statements feel good on their face, even though they are intellectually vacuous. The problem is that Allen seems untroubled by and uninterested in the question of what, exactly, or how, or why this is occurring.
And, so, boringly, on. This book is full of silly arguments. If you’re sensitive to language, your eye and ear will snag on these statements. Their persuasive ability comes from their ability to sound plausible and intelligent and to be quickly forgotten about. It’s a manipulative way to write.
It’s sad because this book has moments of genuine eloquence. To be sure, the book is very personal, very well-written, but it’s also not very exciting. It’s actually quite dull. It’s worth asking yourself: what is Allen telling us here that we don’t already know? What have we learned?
Why should this matter? Because the value in Allen’s “true story about schizophrenia” comes from its power to nurture critical thinking and promote empathy among readers. Allen’s lack of rigor, care, and self-reflection betray an authorial intent that seems fueled by self-interest and exploitation rather than curiosity and care for people with severe mental illness. In this way, Allen’s project undermines both our understanding of schizophrenia and our ability to foster genuine empathy for people deemed to be a less-than-fully human threat to society.
If AKOMP had focused on Bob’s story alone, it would be have been an excellent contribution to the understanding of schizophrenia. So why did Allen step out of their zone of expertise to profile the meaning of schizophrenia itself?
It’s not my place to question the author’s emotional life, and it’s entirely possible that the mistakes made by the author are the result of misinformed or poor research, so let’s skip to another question concerning fact-checking: if this book was fact-checked, why are there so many errors? One answer is that Allen was intent on shoring up a conclusion they had reached well before they began their reporting for this book.
As it happens, Allen considers the kind of pre-mature conclusion bias in the context of making sense of Bob’s life story:
Had I read Bob’s manuscript only up to the description of his first stay at Herrick Hospital, I might have supposed it was a screed against psychiatry as a whole. Or that he disputed the idea that there was something going on inside his brain, something that made it hard for him sometimes. But his manuscript didn’t dispute this; perhaps it’s what he meant when he wrote on his manuscript’s cover page that he was unable to identify with reality.
Indeed, a troubling consequence of the author’s apparent anti-medication position is how it seems to be at odds with the reality of Bob’s life. By all accounts, Bob seems to have embraced medication and psychiatric care, even after experiencing violent and traumatic hospitalization. There’s no doubt about the horrifying description of Bob’s early hospitalization, where he was forcibly medicated and abused by staff. Still, he kept taking his medications, even despite the awful side effects. For instance, at the age of 55, Bob writes: “IM STILL ON MEDS, AS LONG AS THE GOV. PAYS FOR THIS SHIT, ILL KEEP TAKING IT.”
In another example, Allen lumps Bob in with “many people” who “call the diagnosis [of schizophrenia] itself as ‘label,’ a tool used to discriminate against, confine, discredit, and silence.”
Surely, as is clear from context, neither Bob nor Gene defined “label” as “a tool used to discriminate against, confine, discredit, and silence.” Indeed, I would argue that the average person (even “most people”) would understand “label” to indicate a name or category or classification that is someone attached or assigned to a person. This may not seem like a big deal, but I would argue that by overlooking this and letting it slide, the implication is that Allen is a better source, having already provided the word with a specific meaning—one that the reader is invited to fall back on. It doesn’t matter that Allen’s definition may be completely distinct from how Bob understands the term “label” – as a general name, classification, or category that is applied to something or someone, as is implied several pages later when Allen reports that Bob’s father, for whom the diagnostic category of schizophrenia carried little meaning, “also referred the diagnosis as a label.”
I find it oddly unsettling that Allen cannot – or will not – offer any satisfying explanation for writing Bob’s story. The most expansive answers come early in the book, when Allen expands on the process of translating or “covering” Bob’s manuscript:
I wrote my version of it, referencing his account as my guide. I kept going, really studying a chunk of his story and then writing it in a way that captured his spirit as vividly as I could.
Writing this way forced me to read his book closely, to try to understand every single phrase, no matter how seemingly unintelligible. Occasionally, I’d still decide that the way he’d put something was just too beautiful or funny or moving—or profane—to chance, and so I’d leave it his way. The capitalized words and phrases served as reminders, too, that this was someone else’s story.
Allen indicates that their they’ve “never had good answers” when asked what interested them about Bob’s story. It seems like an important question. Allen suggests that a “more interesting question” is why they kept writing, not why they began in the first place. It feels like a fatuous question designed intentionally bring about a particular kind of reading (or misreading). Put differently, Allen’s suggested question seems designed to protect the text from close reading. I could be wrong.
Allen also doesn’t reflect on the ethics of appropriation or their rights to claim authorial control over a story that’s not their own and without the permission of the original author. Allen doesn’t reflect on the representational politics of writing a story from a place of privilege about a topic which with they are self-admittedly (and demonstrably) have little to no expertise in. The utter lack of self-reflection combined with several other things raises a profoundly important question: Is Allen the correct person to write this book?
Here’s my question: why is Bob not included as a co-author to this book? The bulk of the book is his story (as told by Allen). What’s the justification for such a glaring oversight? Allen doesn’t offer any satisfying answers. The best we get is an early passage, where Allen describes writing their version of Bob’s story, “referencing his account as a guide,” with the added assurance that they wrote the book “in a way that captured his spirit as vividly as [they] could.” Yeah, but how? Allen offers nothing.
Finally, did the following really happen?:
I am curious about one particular event from Bob’s life, which I must be honest, reads as being completely made-up. The event in question occurs during Bob’s awful hospitalization and comes after he describes a promise from his friend Bart that, when he was discharged, he would protest their treatment by “going to the press” and telling the world about the conditions of the hospital. The passage, which comes early in the book, didn’t raise red flags at the time since the reader accepts that some of what Bob autobiography entails may be fantasy given the nature of his state of mind. However, in light of Allen’s admission at the end of the book, where they expresses meticulous attention to the factual quality of Bob’s memoir by fact checking Bob’s life details, including his time in the military, where he went to schools, and even verifying his certificate in welding, and then following up all of that by comparing stories and notes with family, something about Allen’s acceptance of Bob’s story of watching television in the hospital dayroom only hours after Bart was discharged only to see his friend on the news, protesting the treatment at Herrick Hospital and speaking to a reporter. Specifically, Allen writes:
That evening Bob was sitting on the sofa in the dayroom. On the news, a big black guy surrounded by protestors was talking into a reporter’s microphone. It took Bob a moment to recognize Bart, in part because he was wearing fatigues, not pajamas.
What was Bart doing on TV?He was flanked by about twenty-five people. They were holding signs; one said SHRINMKS KILL: Bart was yelling something.
It seems relatively easy to verify if it did since it was a televised segment. And given that Allen later describes investigating Bob’s dog to make sure it was real and jokingly attempting to verify Bob’s story about meeting Kenny Rogers as a patient in a psych ward and playing music with him Allen describes reaching out to Rogers, but not getting a response, which conveys some degree of incredulity on Allen’s part, although they do not come out and explicitly express disbelief. This doubt is not present anywhere in Allen’s telling of Bob seeing his friend on television the very day he was released, keeping his promise and whistleblowing on the hospital. In fact, Allen seems to double-down by offering some plausible explanation, perhaps sensing that the reader may harbor doubts, Allen points out that: “The first antipsychiatric protests were held around then, in Berkeley and a few other American cities—which perhaps explains what Bob saw Bart participating in on TV.” For me, the disbelief is based on the wild coincidence that a psychiatric patient would be discharged and able to contact appropriate media people that day and be taken seriously enough to be put on television and then Bob, while locked up in a very rundown and by all accounts abusive psychiatric institution would be watching that television news station that evening at the same time. It just all seems so implausible.
In the previous post, I described an ugly knot of a study from 2017 that centers on how ordinary people, who self-identify with a bipolar diagnosis, narrate their identity and experience through personal blogs. In eight short pages, the authors manage to:
- Deny agency to research subjects with bipolar disorder
- Impose a narrative on every mentally ill person (we are not all the same)
- Present an argument that impacts access to care in a very bad and unethical way
- Claim to know about mental illness from the outside
- Prioritize their research over the humanity of their subjects and others with this diagnosis
Deploying a value-laden methodology, the authors mine, quote, and re-publish sensitive information from personal blogs written by members of a community of which they are not active participants, without informed consent or permission from the bloggers, and for which they do not provide deep context. They consistently choose to ignore the truth from their subjects who write about their life in intelligent, accessible ways that are also brave and resilient.
What makes this study egregious, thought, is how the authors claim expertise on bipolar disorder identity by reducing a complex diagnosis and illness experience to a trivial performance or commodity. For the authors, these bloggers are not just wrong. They lack legitimate grievances.
The authors advance simplistic, moralizing, and claims on their subjects’ motives and character that threaten their reputations, access to support, and increase their risk of harm. Their colossally superficial analysis presents them as weak and amoral people at best; deceptive drug-seeking malingerers at worst.
Rather, the authors gesture toward a mind-bogglingly anodyne debasement of the medical model brought on by mainstream psychiatry’s (increasingly transparent) collusion with “big pharma.”
What’s the point of this?
When I first became aware of this research via twitter, I was horrified. The ethical and moral void, yep. But it would take another month before I read the study for myself, followed by (at least) another month of thinking, reading, tweeting, and writing before I could begin to articulate the depths of my outrage.
Through it all, I’ve been consistently plagued by the same set of questions: Why this study was conducted? Who does it serve? How does its benefit outweigh its horrible ethics, lack of intellectual rigor, and insidious analysis? Is this scholarship?
In the conclusion of the paper, the authors appear to offer a pithy justification for why this research matters, their most explicit articulation in the entire paper. They state:
“Clinicians need to be aware that what patients regard as BD may not correspond to the conditions for which the drug treatment has been tested. The pros and cons of this wider idea of BD require further debate and research.”
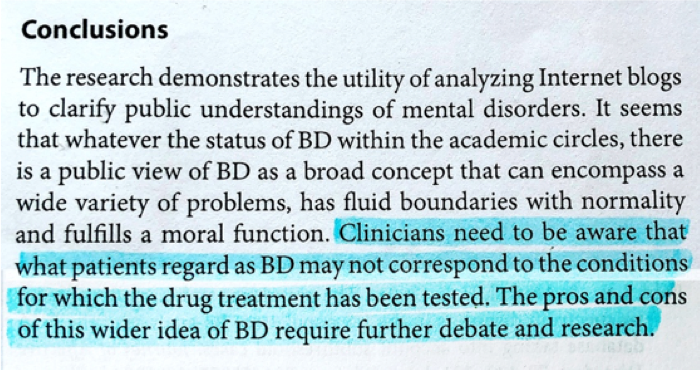
It’s worth a look at the second part of the authors’ claim, which informs the first: that “this wider idea” of bipolar disorder identity deserves “further debate and research.”
“The pros and cons of this wider idea of BD” is premised on bipolar disorder being a voluntary choice. The academic basis for such a claim aside, the authors make a leap from vague observations that their subjects’ narratives are: 1) “consistent with ideas presented on drug company websites,” and 2) “illustrate the attachment…to their diagnosis” to specific—and not explicitly hypothetical—instances of bloggers clandestinely deploy their diagnostic identity for personal gain (“mind-altering” psychotropics and/or money).
Clouded in academic trappings and qualifiers, the authors advance some toxic victim-shaming. The first claim (1) is too lazy to be examined in-depth. The second (2) is much more toxic and patronizing. Providing no evidence, even anecdotally, the authors suggest that bipolar disorder serves a “moral function” that enables sufferers to cling tightly to a diagnostic identity in such a way to cover up their personality flaws and legitimize bad character.
Which, of course, isn’t true. If bipolar disorder is being singularly attached to the subjects in ways that detract from their humanity, it’s because the authors chose to objectify them to tell a singular story. It’s a suspiciously paradoxical claim given the authors’ non-identitarian stance is built into this study. The authors literally designed their research in a way that enabled them to discard the author bloggers—compelling them to assume an almost organic and biological relationship with the media technology they used.
Which circles us back to the authors’ conclusion: the call for “further research and debate.” It’s an argument with a dead end, at the dead end before we even turn onto the road.
There are no “both sides” in a “debate” about whether people suffering from severe mental illness should be believed or exposed to harm with the people who are actively trying to harm them. There is only hatred and bigotry, which is rooted only in lies and misconceptions.
The Bad Faith of Liberal Academics
This study is bad politics and bad faith masquerading as “objective” scholarly insight—bolstered rhetorically via contradiction, sensible language, and the accoutrements of logical thinking. Instead of conducting rigorous scholarship research and attempting to locate a nuanced and more accurate “bipolar identity” in their subjects, the authors relied on value-laden reductionism and oppressive tactics to universalize a “truth” about the community this research is designed to support.
This is the danger when academics and intellectual elites, with all sorts of baggage, are allowed to lead and control radical movements. When the 1% of liberal psychiatry collude with an establishment ideology, radicalness is only aesthetic. Critical psychiatry is all talk and no action: bolstered by superficial social justice performances and neologisms, wherein the community they purport to care about are simply set aside rather than the very heart of the matter. It’s a movement that doesn’t challenge or change any of the underlying social conditions that lead to the acceptance of some people with mental health issues into public life and the criminalization and marginalization of other “less deserving” already oppressed folks.
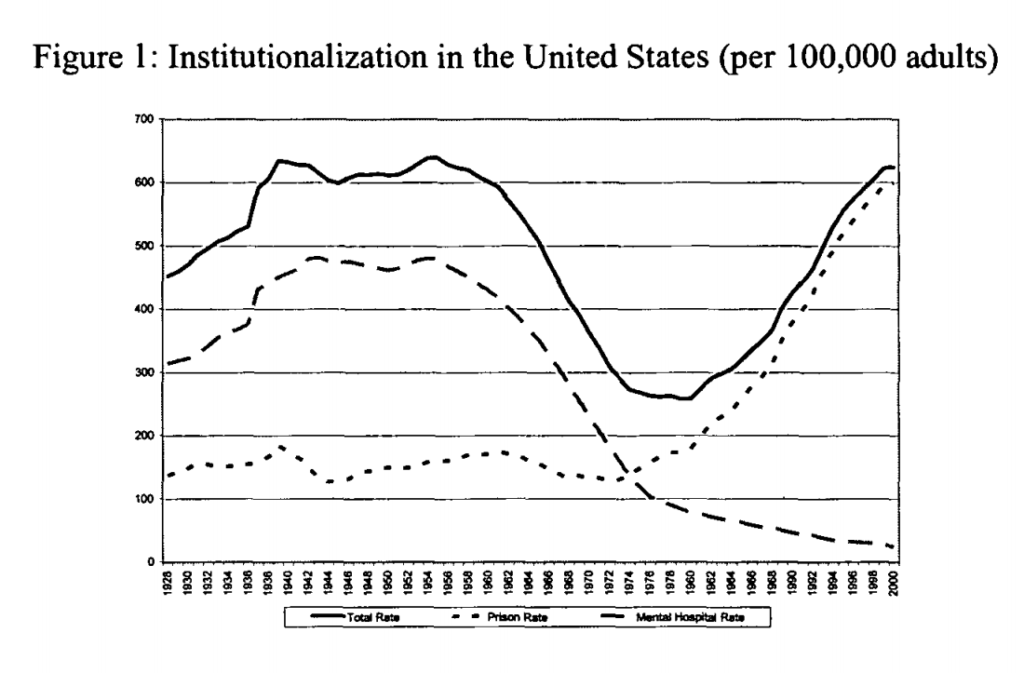
The most marginalized people with mental illness experience more extreme vulnerability, in part because more aspects of their lives are directly controlled by legal and administrative systems of domination—prisons, welfare programs, drug treatment centers, homeless shelters. These intersecting vectors of control make obtaining resources especially difficult, restrict access to zones of safety, and render every loss of job, family support, or access to an advocate or a mental health care more costly. At present, the dehumanizing cells of jails and prisons represent our de facto psychiatric institutions, the long-term psychological effects of detainment on migrant children, the ways in which structural racism and police-perpetuated gun violence exacerbate mental illness.
There’s something very paternalistic and liberal about saving mentally ill people from themselves instead of challenging supremacist institutions. In my mind, the most dangerous psychiatrists and mental health “experts” are not the Szaszian, in-your-face libertarians. It’s the deceptively benevolent ones who couch their ableism and paternalism in fronts of reason, science, faith, and with the guise of “opinion.” It’s centered on exceptionalism and privilege. It’s very Euro-American, it’s very Christian, and it’s very capitalist. “Happiness is a choice! Being negatively affected by racism, sexism, homo/transphobia and poverty are choices too!” Are we going to pretend mental well-being isn’t dependent upon often hostile environmental circumstances or just be reductive and ableist? If you want to put on a perpetually brave face, good for you. But let’s not pretend that regurgitating hypnotic Yoda pseudo-optimism bullshit is universal. As a person who suffers from debilitating depression that renders me non-functional, telling me “it’ll get better” when it’s looking bleak is the worst thing you could do.
Which is to say, if we actually care about justice then we need to find a way to discern people’s intentions before we accept their argument and research as valuable. Harsh as it sounds, there’s no doubt in my mind that the authors intended to humiliate and further alienate, exclude, and stigmatize people who wrote about their bipolar disorder as a legitimate medical condition that required psychiatric treatment via medication. Why? In order(?) to maintain their control over progressive movements, liberal elites must create a diversion to shift attention away from topics that might call on them to engage the messy work of real change. To maintain power, they have to appear busy. A common tactic is to fabricate a threat: perhaps a research study that’s more about separating out intended victims from unthreatened allies than anything meaningful. A red flag is when you find yourself asking, again and again: What’s the point of this? The authors often glide over the answer through rhetorical tics. Thus, they talk of a thing being a “concern” that requires “awareness” and “more research and debate.”
Drawing on my complex experience of “being bipolar” in addition to the original blogs written by the research subjects, I confidently state that next to nothing in this study is valid. It’s an ethical trashfire. I don’t get a choice about “being bipolar” so I’m stuck sharing an identity with the authors of the blogs. But that doesn’t mean I have to tolerate such a harmful study.
When it comes to “being bipolar,” one side is right, and the other side is wrong.
Telling me my identity is bad? Screw you – that’s not a neutral, unharmful opinion. Marginalized identities are not subjective, they’re not “opinions” to be politely debated by White liberal elite intellectuals. Words uttered and written about marginalized identities have an impact on their bodies.
That so many “experts” and academics—including a noted psychiatrist—think they’re qualified or entitled to (un)diagnose ordinary people with serious mental disorders based on a half-assed (or even whole-assed) engagement with a blog is even more reason not to trust anything in this study. No one is qualified to do this, no matter how much training they’ve had. You should be uncomfortable in the care of a mental health professional who has publicly demonstrated a willingness to judge someone, in aid of an ideology or in bad faith, who is suffering with a stigmatized disorder and has left digital breadcrumbs to their offline identity.
You don’t get to walk away from this kind of mendacity, no matter how important you are. Here’s why: it’s symptomatic of an institutional privilege and power whose checks and balances are sick, whose publication review processes are broken, and whose senior experts speak only in terms of what makes good or bad research without any reflexivity or ethical consideration.
Even if you choose to believe that the authors made all of these mistakes, not maliciously, but carelessly: it doesn’t make it any better. In fact, it makes it worse since it reveals a pattern, a habit, a system. The authors wrote with the easy knowledge that they would be believed, that theirs was the definitive and credible word, despite their distance and ignorance from the events in question. They wrote distracted, assuming no one who mattered was likely to question their account. (The bloggers would know the truth, of course. As would others with bipolar disorder. But no one told them about this study and even if they were informed, they have little ability or access to enter the conversation. They are effectively without the right to respond).
I imagine the authors will respond to my outrage in all or none of the following ways:
- Confusion: Why don’t I welcome minority viewpoints that challenge harm and coercion perpetuated by mainstream psychiatry?
- Dismissal: I’m not competent enough to know what’s best for me.
- Hostility: I’m brainwashed by Big Pharma or masquerading as mentally ill for my own personal agenda.
- Complacency: Continuing with what they’re doing because I can’t stop them.
I’ve seen this pattern before. But I should also add “But, academic freedom” and “You’re a conspiracy theorist” to the list to be safe.
Impolite Conversations
In the weeks I’ve been writing about this study, I’ve constantly worried about coming across as a respectful and serious scholar who demonstrates an appropriate “open-mindedness” in public. Gaslighting makes us question ourselves because we’re forced to entertain how academics and entire movements void us of our humanity and our capacity to define ourselves as equals.
The choice to engage in one-sided dialogue with power requires a lot of mental gymnastics. As such, there’s a tendency to self-police so as not to be too threatening, or an attempt to center and accommodate the feelings of the oppressor so that our humanity becomes easier for them to understand. I’ve written many drafts of this blog. It’s even easier to abandon a justifiably militant position in favor a more respectful one or silence simply as a means of coping over the seemingly never-ending demands for our rights to existence and freedom from violence.
But if we truly want less ableism and bigotry towards mental illness, we need to show that ableism and bigotry are unacceptable and beyond the pale. Civil conversations that concede virtually everything are not the way to get there.
There’s no justification for continually discounting the testimony of people diagnosed and/or suffering from serious mental illness other than to call it out as ableism and paternalism and question the motivations and credibility of the researchers who do this work.
Given what we know about this study and the authors, this is an easy call to make.
This research must not only be stopped; It must also be atoned for. The authors must acknowledge the harm they’ve done.
Why do they need to do this?
To be damn decent people for one. But in a practical sense: because people who identify as having a mental illness are the backbone of any meaningful understanding of where our problems started and what it will take to resolve them. And they don’t have a lot of our trust. Without us, the authors’ privilege will let them publish books and articles and secure speaking gigs, and be the face of a movement, but it won’t galvanize any actual action. It will generate personal power, but it won’t uplift the people they’re purporting to help.
Personal blogs are an act of communion, an act of humanity, the sharing of your story with another person. We each contain within us a private cosmos, and when we write ourselves, we make visible the constellations that constitute our experience and identity. However, there are many ways that these stories can lead to harm People who blog about mental illness are vulnerable to many types of harm, and unfortunately, sometimes those harms come from their “allies.”
Nowhere is this made more evident than in the article “Being Bipolar: A Qualitative Analysis of the Experience of Bipolar Disorder as Described in Internet Blogs,” published in the Journal of Mental Health Nursing in September 2017. This qualitative study—lead by renowned psychiatrist Joanna Moncrieff with Anika Mandla and Jo Billings—analyzed a small sample of personal blogs written by self-identified bipolar disorder sufferers.
The authors in this study—authoritative, supposedly impartial and identity-less—undertook a thematic analysis of relevant material in personal blogs about the experience of bipolar disorder, including blogs from bipolar blogging networks, and critically examine the arguments used in support of and in opposition to mainstream conceptions based on the medical model. In reality, this research reflects a tremendously unethical, exploitative, co-option by the authors—insidiously occurring under the guise of welcoming and embracing knowledge.
Stories about mental illness belong to different domains of experience, but they have one thing in common: the people they belong to are seldom engaged with as authentic and credible thinkers, philosophers, or experts. While no means unique in its use of social media for data mining, this study functions as an up-to-date exemplar of vapid online research practices concerning marginalized groups.
Why “Being Bipolar” is Such an Unethical Study, And Why We Should Care
Let’s begin with the most succinct and disturbing sentence of the study which clarifies the authors’ cavalier approach to ethics:
“Ethical approval was considered to be unnecessary given the blogs are publicly available, but all quotations have been anonymized.”
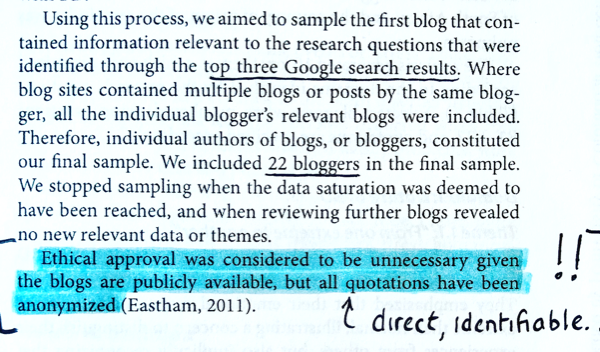
As a careful reader, you might well be wondering how one can anonymize direct quotations, and the answer is: you can’t. There’s no such thing as an anonymized direct quote of an internet source. What the authors have done is merely produce an illusion of anonymity, and they’re done it poorly. The decision to pseudoanonymize subjects might be anodyne, but it also seems to indicate that the authors were not fully invested in their belief that personal blogs on mental illness are entirely of the public sphere.
There is much disagreement on whether content on publicly accessible personal blogs should be considered as freely available for any researcher to use. On the one side are those who take an almost laissez-faire view and see anything published on blogs as “fair game” for research purposes. Inherent in this view is the belief that authors have no reasonable expectations of privacy. On the other side are those understand that digital technology and culture have blurred the boundaries of privacy requiring more nuanced, fluid, and contextual conceptions.
The authors are in the first camp. They take an individualistic approach to privacy, despite the fact that, historically, socially, and politically vulnerable subjects haven’t been granted the same “right” to privacy as dominant groups—either offline or online.
They consider bloggers to be ultimate arbitrators of their fate, fully assuming all concurrent risks and potential harms that may come to them since they made the decision to post sensitive data in a publicly accessible space.
By this logic, bloggers with mental illness are not only responsible for paranoid caution and isolation from online communities, but the perpetrators (the authors) themselves bear no responsibility for predatory behavior. That kind of logic is how the criminal justice system falls apart.
“It isn’t the burglar’s responsibility for robbery if you didn’t exercise due diligence and hire a guard or invest in a security system.”
“We can’t try this murderer because you didn’t wear a bulletproof vest and helmet when you left the house this morning.”
The belief that individuals are responsible for the overcoming external harms levied against them is a theme throughout this paper.
The Worst Myth of Mental Illness
Running alongside this rejection of an ethical obligation to protect their subjects, is the authors’ sanctimonious, distorted, and offensive characterization of their blogs.
First up is the moralizing. According to the authors, a professional or self-imposed diagnosis of bipolar disorder is “real” in the biological sense but as functions morally in ways that enable “people to extrude unwanted parts of their personality into their ‘illness’.” In other words, when it’s taken up or diagnosed as a legitimate psychiatric disorder, “bipolar identity” is nothing more than a weakness of will; a crutch sufferers use to obfuscate “extreme, bizarre, usually dysfunctional and sometimes unfathomable manifestations of human agency.”
This is a bold and sanctimonious stance. The basis for a person’s character flaw? According to the authors, it can be gleaned by how bloggers attach themselves to their diagnosis.
The thing is, though, mentally ill people aren’t the ones making ourselves all about our illnesses. It’s people like the authors who choose to decontextualize and extrapolate from blogs about mental illness that make us all about our illness. In the context of this study, the experiences penned by bloggers who self-label with a “bipolar identity” are invented out of whole cloth, with no apparent connection to the circumstances of their lives—presented without race, class, gender, sexuality, or disability. The testimony of their lived experience is disembodied, decontextualized, and misrepresented by the authors with the assumption that these blogs reflect a consistent singular identity within and across bloggers.
Scientific Merit
Obtaining quality data and analyzing it properly is an essential component of ethically defensible research. Unfortunately, the authors seem to have gotten short with the truth and have interpreted bloggers’ words in value-laden and irresponsible ways.
Consider the following interpretation, extracted from the paper:
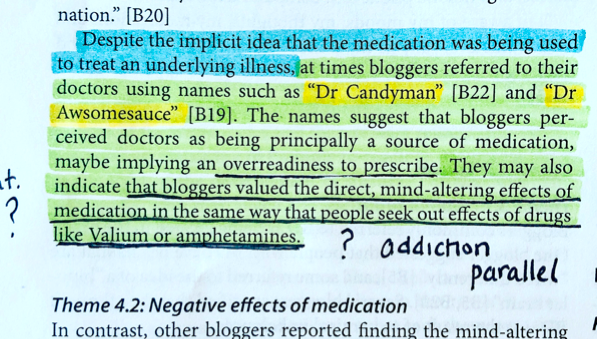
“Despite the implicit idea that the medication was being used to treat an underlying illness, at times bloggers referred to their doctors using names such as “Dr Candyman” [B22] and “Dr Awesomesauce” [B19]. The names suggest that bloggers perceived doctors as being principally a source of medication, implying an overreadiness to prescribe. They may also indicate that bloggers valued the direct, mind-altering effects of medication in the same way that people seek out effects of drugs like Valium or amphetamines.”
Oceans of contempt and nonsense, all wrapped up in three sentences. I’ve read the blogs from which these quotes are taken and they do not “suggest” or “indicate” any of this.
The word “awesomesauce” (extremely good; excellent) was officially added to the Oxford English Dictionary in three years ago. Before that it held the same meaning as lighthearted slang. In the original entry, Dr. Awesomesauce exists in relation to Dr. Goodenough, and the author is hyperaware and concerned with being overmedicated. Of note, is the reference to an internalized stigma due to feeling like a “personal failure” for needing an antipsychotic.
While Dr. Candyman may seem like less of a stretch for describing an over-prescribing physician, the context of the entry is important. Here, the blogger is writing about two providers: psychiatrist (Dr. Candyman) and psychotherapist. More importantly, Dr. Candyman is described as providing helpful advice in finding a therapist. There is not a single mention of medication. The reasonable conclusion is this is lighthearted, sarcastic nickname for a medical doctor.
Let’s be absolutely clear about what’s happening here: the authors’ presented two bloggers’ nicknames for their psychiatrists and drew a straight line to a celebration of medication. This magnificently premature and misleading. They then make an interesting parallel to addiction and end with the conclusion that these bloggers may be opportunistic junkies.
The message is clear: these bloggers are manipulating a diagnostic identity in order to get drugs (which by their accounts made them feel terrible). We can take this even further to suggests that people with bipolar disorder disobey an authority and a legal system already in place to obtain “mind-altering” drugs that they don’t really need. The implicit assumption is that these bloggers might be criminals—in a judicial system already betrays people it purports to protect against racist, ableist, and classist favoring.
I am frustrated at the authors’ insouciance. Their cherry-picking for punctiform one-liners and contrived examples. These matter-of-fact assertions of less-than-obvious generalizations absent any elaboration are patterned in strange and increasingly troubling ways culminating into such a cataclysmically myopic paper. This is shameful. These quotations are embodied and situated in deeply authentic narratives that belie any of the authors’ defamatory and unprofessional interpretations/conclusions.
If you attribute an individuals’ character to her mental illness, you’re placing the responsibility for its existence squarely on her. It isn’t an oppressed person’s duty to survive and shoulder responsibility for mental illness. That idea itself is violent. However, the authors take their gaslighting much further by enacting violent and disciplinary reactions to their subjects.
Fake News
Donald Trump’s deployment of “fake news”—an abusive static logic that combines habitual lying, invalidation of trauma, a refusal to be held accountable for his statements, and skepticism of the media—presents a clear example of gaslighting in action. But Trump’s use of false rhetoric has been well-covered. More subtle yet nevertheless insidious is the gaslighting performed by the Moncrieff and colleagues, and those who defend their claims. The authors, for the most part, have been widely-revered by cis white middle-class Eurocentric circles, treated as renowned scholars, radical advocates, or personal heroes than the embodiment of harm.
The authors’ conviction that bipolar disorder is not only over-described and over-prescribed, but also not a “real” bodily illness at all, is a belief that brings them into direct opposition with the experiences of their subjects. Nowhere is this more apparent than the authors’ skepticism and credulity about the motivations of those who write about their experiences with mental illness (and blogging) is described in the following excerpt (emphasis mine):
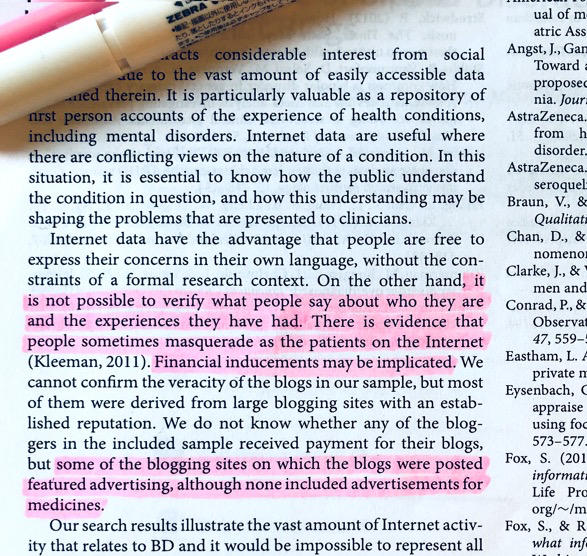
“Internet data have the advantage that people are free to express their concerns in their own language, without the constraints of a formal research context. On the other hand, it is not possible to verify what people say about who they are and the experiences they have had. There is evidence that people sometimes masquerade as the patients on Internet(Kleeman, 2011). Financial inducements may be implicated. We cannot confirm the veracity of the blogs in our sample, but most of them were derived from large blogging sites with an established reputation. We do not know whether any of the bloggers in the included sample received payment for their blogs, but some of the blogging sites on which the blogs were posted featured advertising, although none included advertisements for medicines.”
To sum up: they illustrate how well they listen to their subjects: the authors first suggest they aren’t even real people, then suggest they are acting deceptively by faking their distress for attention or personal gain (supported with a citation for an article on Munchausen syndrome, itself a psychiatric diagnosis for people who “play sick” for sympathy or attention). All the while, they cite the motive for profit as if to imply that writing deeply personal illness narratives on bipolar disorder blogging networks is a lucrative venture.
If the authors are studying the representation of “bipolar identity” on blogs written by self-described sufferers, then how are concerns on “fake distress” and “malingering patients” even relevant? For instance, even if a person is choosing a fictitious identity or creating a fictitious literary narrative, the desire is real and culturally significant. The authors seem to state this themselves in the next paragraph where they justify the importance of their research, as depicted below (emphasis mine):
“[S]ince the included blogs were easily accessed, whether or not they were genuine or representative, their content is important because it is likely to exert a disproportionate influence over public views.”
It’s one of many interesting contradictions and rhetorical moves in this study. These aren’t mistakes. This is deliberate and formulaic; they are following an unoriginal pattern of omission in order to misrepresent. Bourgeois academics like Moncrieff are deliberately vague, elaborating as little as possible and often time not at all. The contradictions are tactical and instrumental ways to direct a particular narrative. On the one hand, we’re meant to blame the bloggers for being manipulative and to sympathize with the authors (the obvious subtext). But the ending context about mental health stigma and discrimination was somehow not connected to the story at all?
The takeaway from this is for “normal” people to be skeptical of people with bipolar disorder for their “mental illness deception,” especially within a binarized and medicalized space, not a nuanced and balanced piece of straightforward reporting about blogs and identity. This is gross. This is harmful and amoral research that also lacks any validity or utility since the data analysis is inflected with the authors value-system.
Everything about this study is condescending and invalidating. The intellectual and practical dangers in this bootstrap rhetoric and moral model approach to mental illness reflects the same problematic logic of the medical model. They both employ the same oppressive logics to pathologize suffering and locate deviancy within an individual. Both perceive suffering and distress as “all in one’s head.” Both are harsh on the individual and soft on the social. This can be most clearly seen in the way the authors’ question the legitimacy of bloggers suffering: a move that only makes sense when you evacuate the politics of now from culpability and place the onus of well-being squarely on the individual.
What a lot of victim blaming and shaming people don’t understand is how mentally exhausting it is to never stop blaming yourself for your victimization. They don’t understand how terrifying it is to enter a space and be hyper-vigilant because you are solely responsible for the harm that befalls you. The internalized shame, guilt, and external shame that comes with consuming psychiatric medication is not unfamiliar to anyone with mental illness, including the bloggers under study.
At the risk of making this too much about me, I need to make my beliefs and reasons clear, such as they are (and were):
- I suffer from schizophrenia, or, as the authors of this study put it, “no I don’t.”
- I don’t like being spoken for.
- Whenever I hear the “mental illness is a myth” song, my ears shut down. I do not agree with the reasoning or the world view it produces.
- I do not believe that mental illness is a character flaw or a moral thermometer (but being sanctimonious and condescending toward people with mental illness/accusing them of faking for attention certainly is).
I know from experience that when I stop taking my medication I cannot function: I cannot move and no amount of validation, hugs, therapy, yoga, or aromatherapy can change that. That’s just me. I do not take my medication to get high; I just want to not kill myself. Like many people, I hate being on them. Relying on potent, mind-altering substances to function produces no small amount of shame, not to mention existential anxiety. I’ve tried to go off them many times in the hopes that the “real me” will finally be able to stand on her own. Each time, I run into the heartbreaking reality that my unaltered self is too painful to bear. This is not theoretical. I know this subject.
That said, this need to be said too: I’ve become perceptive to academics who appear to be doing the right thing while leveraging trauma for gain. Again, this is gross. And inexcusable.
Reimagining Ethical Research Online
There’s an urgent need to recognize the ways that we as researchers of vulnerable and stigmatized subjects reproduce and escalate harm and capitalize on (rather than care for) sensitive and identifiable data. This requires reflexivity at every step.
Water (and cats) flow into the shape of their container. And the internet has vastly changed the shape of the container. Our lives are contoured to the unique contexts into which we are born and reside which themselves shape our actions, emotions, and mindsets. Personal blogs and social media change the way we build relationships, share information, and make everyday decisions, including decisions about health and wellbeing.
It seems that many researchers want to find the “right way” to conduct research, by which they mean they want to check a bunch of boxes that will reassure them that it’s allowed and passable, without considering the possibility that maybe they just don’t do the research. There is a kind of colonial/white supremacist (and I think deeply patriarchal) stance which presumes that everyone ought to be able to study everything and I just think that all arguments that proceed from that premise are deeply flawed.
We need to understand that not every blog post or tweet is “for” us just because we can access it. We aren’t always the audience and therefore don’t always deserve extended explanations or history/context we’ve missed. When the content is of a sensitive or risky nature or involves marginalized identities, we need to consider whether we have a right to research at all.
Careful and respectful research can be done in ways that produce valuable knowledge, but they must foremost be motivated by an ethical commitment to participants and the desire to respect their knowledge and experiences. De-anonymization, the phenomenon of doxxing, harassment, and stalking are all live and urgent concerns on social media. It’s upsetting that our society and culture contains a seemingly endless supply of ways to make marginalized people feel unsafe and unwelcome. On the flipside, online spaces are emancipatory too. But it must be understood that public information exists in the context of power and consent, and we must construct our ethics in that context. The impulse, when an encounter between a human and theory goes badly, is to extract a lesson, but what moral can you draw from an encounter like this? That will be explored in Part 2.
Preface
(This is not going to be a very good blog post but it will be very long).
Why do people consider Derek Jeffreys’ book America’s Jails “groundbreaking” and “rich and thoughtful”? Why is it considered to be “a powerful condemnation of America’s jail system”? (This ebullient praise comes from two quotations on the back cover by reviewers who I assume either share the same fanatical politics as the author; or didn’t bother to read the book).
I find it disgusting, and I think this is the best thing you can say about it: this book should have never been published. In a disjointed fumble of personal anecdotes, aggressively irresponsible rhetoric, and hollow philosophical analysis, Jeffreys has written a book that centers the redemption and goodness of the cops and prison guards who harm as opposed to their victims. It’s a book that doesn’t even try to hide its white nationalism.
The fact that it’s so terrible in all possible ways – quality, politics, ethics – can’t explain why it was published by New York University Press as non-fiction polemical “alternative criminology” book alongside such luminaries such as Michelle Brown (The Culture of Punishment, 2009) and Judah Schept (Progressive Punishment, 2015). For this reason, it’s worth examining the sophisticated and concerning methods employed by this book in some detail in order to de-mystify—that is, to lay bare, the underlying ideological terrain.
Coping to Some Personal Bias
I wanted so much to like America’s Jails – nay, love it unabashedly. I chose to review this book, based on the descriptive blurbs from the author and publisher; I didn’t privately contain my excitement when I finally received my free copy from the publisher. The topic is close to my heart.
Inevitably America’s Jails sent me on a trip down memory lane. As it happens, I have passed through courtrooms, jails, and forensic state hospitals on my way to who I am today. I have known—personally and intimately—women (and some men) who live their entire lives with one foot to either side of the law. And, in my mind’s eye, I can envision voiceless and despairing people—perpetrators and victims alike—who would hope that a book claiming to “center their inherent dignity” to “shift public perception and understanding of jail inmates” by “highlighting the experiences of inmates themselves” would, well, actually do that. The result did not just disappoint me, it triggered my moral aggression.
Notes on America’s Jails1
My review of this book will be published soon on a website that’s not mine and have decided to post my many, many notes of this book so as to cover my ass lest anyone choose to accuse me – a lowly independent scholar – of being unfair or unrigorous in my critique of this book and the author who wrote it. I am very scared of being wrong here therefore I am dumping a lot of stuff here – in way too much detail – for the purpose of being respectful, comprehensive, and precise.
These notes are divided into sections and do not follow a continuous narrative. I’ve tried to organize everything as logical as possible – in an order that is, more or less, global to local.
- Not-So-Good Intentions
- Conceptual Framework
- Close Reading: Perspective and Representation
- Reparative Reading
Not-So-Good Intentions
This book raises key issues related to authorial intention (political motivation, personal involvement, questionable morals) and the narrative reliability (lack of expertise, unmet promises, false premises, inaccurate representation of fact and fiction).
In this section, I will begin with an attack on the author’s ethics by suggesting his repugnant political and religious motives have produced a book that best belongs in the genre of “fake news,” as defined by Jeremy Geltzer to mean “the publication of knowingly false, deliberately misleading or purposefully manipulated content intended to influence the recipient of the information” (2018, p. 298). The basis for my claims are anchored in a detailed examination and close reading of book – paying attention to methods, style, form, evidence.
About the Author
Jeffreys’ education and professional background is highly relevant to his writing in this book.2 According to his personal website, Jeffreys currently holds the title of Professor of Humanistic Studies and Religion at the University of Wisconsin, Green Bay. He has a PhD in “Religious Ethics” from the University of Chicago Divinity School. However, more interesting is Jeffreys’ undergraduate degree, earned from the University of Chicago in 1987, in a then brand new major called “Fundamentals: Issues and Texts.” Co-founded by Allan Bloom, Leon Kass, and James Redfield, this self-directed program (which is dubbed “fundies” by those in its inner circle) was designed to allow students to research fundamental questions about human existence (e.g. “what is freedom?”) or phenomena such as “what is the purpose of jail?” (which happens to be the eponymous second chapter of Jeffreys book) that held personal interest for them and then spend the next four years seeking answers through a handful of readings of a handful of classic texts of various genres (literary, religious, historical, and philosophical) that were informed by similar question. Outsider of the academy, Jeffreys spent time in the US Army. He has also spent a decade volunteering in prisons and jails throughout Wisconsin, both in the prison chapel and also teaching prisoners “about religious and philosophical topics like evil, anger, and love” (p. 4).
Intended Audience
The back cover tells us that it “aims to shift public perception and understanding of the jail inmates to center their inherent dignity and help eliminate the stigma attached to their incarceration.” I take this to mean that it’s intended for a wider (and whiter) audience of policy makers and the public alike, particularly in a political environment favoring privatization.
Faux Reform
America’s Jails is a form of faux reform that, on the surface, looks promising, but upon closer reading, reveals the author’s deep unwillingness to challenge the existing system. Throughout the book, Jeffreys masquerades as a progressive scholar making a progressive argument by deploying the very same talking points of faux progressive politicians who advocate for criminal justice reform but also seek to fund new jail projects.
In a context where “criminal justice reform” has solidified into a bipartisan issue; becoming trendy enough to be officially endorsed by our very own white nationalist and rapist in a sagging spray tanned pig skin president, there is a new wave of “faux reform” or faux progressive writing creeping into the conversation that, on the surface, seems to be promoting social justice measures but is actually nothing more than old wine in new old bottles. Jeffreys narrow focus on reforming jails does nothing to address the racialized violence of policing nor the structural racism, poverty, and economic violence that produce mass incarceration. Furthermore, Jeffreys’ focus on the structural internal conditions of jail – filth, ugly buildings, broken toilets, lack of beds – combined with concerns about overcrowding provide a perfect foundational argument for advocating for more jails, not fewer. Importantly, this is antithetical to Jeffreys claim that jails are morally unjust but a tragic fact of life (a belief that should be questioned and, ideally, resisted at all costs). But even if the author is acting in good faith: that he does believe jails are morally unjust but a tragic fact of life in order to protect society from the most dangerous and evil criminals; for Jeffreys these are probably serial killers but his focus in distinctly on rapists, child molesters, and domestic abusers. But this is a position that the majority of society, liberal and conservative alike hold – and therefore his argument, at best, suffers from a lack of imagination and resigned hopelessness, what on earth are we to make of an argument that mirrors the very same talking points of many conservative proponents of “bipartisan criminal justice reform” who seek to fund new jail projects by focusing on the conditions of jail, emphasizing the need for improved conditions for those living inside.
The clearest evidence that this book is a fake thing pretending to be real is to look at the policies that Jeffreys proposes. So, what exactly, is Jeffreys seeking to reform? In Chapter 5: “What Can We Do? Responding to a Crisis,” Jeffreys introduces what he considers essential responses that warrant immediate implementation to our “broken system,” including attention to:
- Pretrial risk assessment
- Money bond reform
- Use of force policies
- Improved mental health intake procedures
In other words, his focus in this book is on jails which makes sense given the title. Yet, for a book called America’s Jails, Jeffreys betrays a remarkable lack of understanding about them. In fact, the book’s promising title and aims as laid out on its back cover and within the introduction are completely nullified by the authors’ motives and intentional misrepresentation of jails in a way that mystifies their connection to a larger system of mass incarceration. In other words, Jeffreys conflates mass incarceration and jails routinely – at the same time, he makes technically true and important distinctions between jails and prisons which operate differently – especially in regards to money bond and mental illness (although, this is less the case when one considers how that prisons are also handling their own mental health crisis). What Jeffreys gets wrong about jails is crucial – failing to ignore their connection to a larger system of mass incarceration – which includes state and federal prisons and immigration detention facilities; all of which are inextricably tied to traditional policing.
On some level, Jeffreys knows the distinction between jails and prisons doesn’t matter since he routinely uses the term “prison reform” in the context of his argument about jails. But his proposed short-term solutions apply exclusively to US jails, which exclusively target pre-trial practices and the money bond system, oversight and procedural tweaks including improved intake procedures for mentally ill inmates and strongly worded guidelines about staff violence from the Department of Justice that “prohibit the use of force as a means of retaliation, control of movement, or punishment” support the “timely reporting of inmate abuse.”
Most appallingly, Jeffreys insists that systematic abuse and violence against prisoners in jails must be fixed through “greater jail monitoring, more federal oversight of jails, investigative journalism, and legal challenges from organizations like the ACLU” (p. 13). At the time this book was published, the DOJ was being run by Jeff Sessions, an ardent supporter of harsh sentencing policies, expanded incarceration, racial profiling, and unbridled police power. Jeffreys doesn’t mention any of this or bring up the politics of the current administration or the fact that the Department of Justice for whom he advocates to oversee his short-term solutions. This is all intentional. Jeffreys wants the reader to think he is above petty fighting among “political pundits” on both sides of the aisle. But his anti-politics are actually much worse than that: fanatical, orthodoxical, right-wing, evangelical, and scary as hell.
That Jeffreys frames his short-term solutions as being valuable for their ability to illicit broad political support (p. 11) is a big red flag that doesn’t bode well for any social justice approach, particularly now when we are contending with a rapist in the highest office and another on the supreme court; both of whom rose to power on a wave of right-wing populism defined by a toxic blend of White nationalism and racialized rage. Still, Jeffreys insists that there are deep divides among the political left and right when it comes to this topic. This is a bold faced lie. We can be generous and assume he is (a) delusional and uninformed, which may work since he does admit early in the book that he does not follow these debates closely, which begs the question of why he is writing a book about subjects matter that he is only tenuously familiar with and also telling the reader that he holds all the answers. Similar to Trump, a lot of what makes this book hard to read and also difficult to address is how contradiction and inconsistent it is.
Faith-Based Initiatives
The type of bipartisan reform being pursued by Jeffreys is inextricably tied to the 1990s “welfare reform,” which say “both sides” of the political spectrum coming together in an effort to overhaul a complex system. Of particular relevance, this period say the implementation of faith-based initiatives that resulted in many government-operated welfare programs being replaced by conservative Christian organizations. These initiatives also had criminal justice components, as noted by Kay Whitlock. For example, in 1997, the global prison ministry, Prison Fellowship – which has since become one of the largest programs of its kind – became involved with an evangelical residential pre-release program. Since then, there has been a rise and institutionalization of faith-based ministries in US jails and prisons. Moreover, states began allocating money to these private groups for Christian-centered faith-based programs in jails and prisons. According to Whitlock, these new streams of funding have “justified deregulation on the basis of religious freedom.” Thus, attendant with the agenda of “faith-based” corrections is a lessening of government responsibility for social welfare and an attribution of immorality as the ultimate causes of poverty and crime.
I am not an expert on this matter, but a quick cursory google search of “faith-based prison reform” brings up a page from the Charles Koch Institute for a session that includes CEOs and Executive Directors of the Justice Fellowship and Faith and Freedom Coalition. Just skimming, the phrase “human dignity” jumps out and feels, gut level, very parallel to this book.
I have a theory regarding Jeffreys’ personal involvement… I for one would like to know the nature of his volunteer work in jails and prisons for ten years. I originally assumed it was through his university, but I have a feeling it is with a for-profit faith based ministry. Disclosures of that nature are critical in a book about ethics. If I am right…
Conceptual Framework
America’s Jails belongs to a class of books that carefully straddles the line between two different meanings. The result is essentially two different books: one that claims to center the humanity and dignity of prisoners and one that illuminates their pathological criminality through the emotion of disgust.
- Double Concepts: Dignity and Disgust
- The Objects of Disgust
- Conceptual Incoherence
- More Disgusting Stuff
- Final Comments
Double Concepts: Dignity and Disgust
Just as this book is not really about the lived experience of prisoners, it’s also not really about dignity – at least not as it contributes to the stigmatization and dehumanization of its prisoner victims.
Long Story Short: America’s Jails renews a controversial philosophical debate concerning the function of disgust an indicator of a deep moral response by using jail – and, by extension, the prisoners inside – as philosophical tools to re-center the humanity of the author as well as the humanity of prison guards and cops who enact political violence against the vulnerable.
In this book, Jeffreys proposes an ontological shift, a new orientation toward old values that mirrors American and Puritanical tradition by linking an ideal concept of “human dignity” to the power of the “affective sphere” to insist that “negative affective responses” such as disgust (and its kin: contempt and fear) are highly cognitive emotions that play a central role in our societal impulse to stigmatize and dehumanize current and former prisoners. That is, prisoners are dehumanized – stripped of their personhood status and rendered objects or things because of (a) the ugly aesthetics and horrific sanitary conditions of jails; as well as their “spoiled identity” (á la Goffman) via their status as “criminals.”
Jeffreys insists that the disgust of jails – the degrading living conditions – and the contaminated status of prisoners “naturally” breeds contempt for them by prison staff and the rest of society. Contempt is defined as the experience of feeling “superiority over the disgusting object” (p. 108). In a complete lack of political ethics, Jeffreys argues that reflexive disgust leads to the systemic physical and psychological violence directed at prisoners by cops and guards. Basically, prison personnel abuse, neglect, and murder prisoners because they are disgusted by them and this disgust is completely natural.
It’s a disgusting argument.
But it’s not only disgusting because Jeffreys provides no sustained analysis of the operations of dignity and disgust that would help to convince the reader that these concepts would be ethically directed at protecting the dignity of prisoners than weaponized by those in power to maintain a culture of abuse and degradation against unpopular people who make them uncomfortable; it’s disgusting because of the remarkable ease it so perfectly crystallizes every revolting thing about this book that belongs in a moral landfill twenty thousands leagues under the sea.
The ease between disgust provoking contempt and anger toward the most vulnerable is not only a discursive mark of being dangerous, but also a very dangerous position in which to be. A loss of dignity transforms prisoners from people who possess an inherent goodness with unique capacity for growth and “transcendence” into objects or things that are susceptible to coercion and control and violence. The message is clear in context: the conditions of jail deny human dignity; foul odors, filth, loud sounds, exposed, malfunctioning toilets, overcrowding, lack of facilities, shortage of bed, ugly buildings, rodents, sick prisoners, bodily fluids, bad smells, loud noises. Within the jail, prisoners are non-people, monsters who must be defended against. Therefore, any violence from these non-people must be mitigated and defended against through the use of force given their dangerous status and is therefore justified in the name of public safety. I’m not sure that makes sense but the point I am trying to make is that Jeffreys has set-up a conceptual framework that essentially “traps” prisoners into a state of perpetual thingification. The key to doing this, I think, is by refusing to blame or hold accountable the cops, guards, and staff who assault and neglect prisoners on a daily basis. The only way Jeffreys can do this is by making an argument that their violence is somehow “natural” or beyond their control.
Definitions:
What is Dignity?
Dignity is a thorny concept. Jeffreys defines an ideal of dignity as the “value of a person” (p 79). What is a value? “Values are what attract us and gain our attention” (p. 79). So, dignity has something to do with values, which are whatever the what that attracts us to another person is.
At the same time, Jeffreys invokes the same term, but time as a verb, to show us how to value someone else’s dignity. In particular:
- “[w}e ought to be attention to the inner lives of those we confine and consider how our practices devalue their individual identity” (p. 96).
- “[w]e should refrain from treating them merely as things or commodities” (p. 97).
Then, to value someone’s dignity involves recognition of their “inner life” – their individual identity – which is presumably accomplished partly by not “thingifying” or commodifying them. And yet, Jeffreys clearly hasn’t done the reading since within the prison industrial complex, prisoners are commodities just like computers and corn are commodities.
As we read on, we learn that we possess dignity “because of our reason and autonomy…and our transcendence in relation to values” (p. 82).
I am not clear on what “transcendence” means and Jeffreys doesn’t provide a clear definition. It seems super religious-y. In my mind, I have been thinking about it as a vague destination that comes from “growth” – whatever that might be. However, we learn that inherent human dignity is tied to rationality and our capacity for self-determination.
Which…is interesting given that incarceration, by definition, removes individuals from the autonomy of their private lives and places them at the mercy of the state for the purposes of punishment. Incarcerated people, therefore, are completely reliant on the state to meet their basic needs. In the absence of the fulfillment of those needs, illness, pain, or even death can result. Jeffreys doesn’t address any of this.
Moving on, Jeffreys draws inspiration from Erving Goffman’s notion of stigma as a “spoiled identity.” Jeffreys tells us that “[s]tigma involves a failure to recognize a person’s individual identity” (p. 102). Furthermore, we are told that we can know perfectly well that a person has dignity and still stigmatize them. How so? Because the ugly aesthetic and degrading conditions of jails fuel “negative affective responses” like disgust, contempt, and fear “blind” people including prison guards and staff to a prisoner’s inherent value as a person.
In a complete lack of political ethics, Jeffreys invokes an ableist concept of “value blindness,” which he defines “an incapacity to recognize the centrality of a value” (p. 100), to argue that “disgust and contempt lead some staff to abuse inmates” (p. 100).
This wasn’t the book I wanted to read. I certainly wasn’t expecting a “captors don’t abuse vulnerable bodies, philosophical concepts do” argument. To be clear, I think this is a ludicrous load of ideology.
The Objects of Disgust
No other part of this book makes me sigh and give up faster than the conceptual “bit” — which, to be completely clear, is saying something. I confess, to begin, that I cannot get a firm grip on how all of this works, or what the hell is going on philosophically. So, I am least confident – and least motivated – to untangle this mess. But, that said: I am confidently sure this is all garbage.
The primary emotion featured in text is disgust.
Definition:
What is Disgust?
Jeffreys defines disgust as “a reaction to something we think is contaminated and inappropriately located,” arguing that disgusting objects “often culturally-specific, and include putrified objects, insects, bodily secretions, dirty bodies, kinds of foods, and forms of sexual activity” (p. 100). Here, he seems to conflate conditions characteristic of the contemporary world with conditions common to all human societies.
According to Jeffreys there is also a moral component to disgust that relates to the topic at hand since “we find vices and crimes disgusting” (p. 105).
Jeffreys provides the example of child molesters and how “many” people find them and their crimes disgusting. In addition, Jeffreys notes how in the past, many have also found certain groups disgusting, writing:
“This deeply problematic kind of disgust often persists despite arguments demonstrating its irrationality. For example, disgust at Jews in some societies has often endured despite its unethical and irrational character” (p. 105).
Jeffreys’ approach to “ugly” emotions and their “objects” is inextricably tied by to the early 18th century “realist phenomenology” of Very Catholic philosopher Aurel Kolani. According to Kolani – and, by extension, Jeffreys – “negative affective responses” are the means by which the human mind apprehends certain qualities about the world, most importantly, those qualities that pertain to the (dis)value of objects. The primary emotion discussed by in America’s Jails is disgust. Emotions also have intentionality since they “reach out” towards their objects. In this case, intentional does not refer to purpose or deliberate intent but rather to the fact that mental phenomena such as disgust, contempt, and fear are “about something”; they are directed towards some object or another. (So, if I am disgusted by spiders or prisoners or gay people, my fear is directed towards spiders, prisoners, and gay people, and they are its intentional object. Of course, all of this raises the question of whether people might set out to disgust themselves. Or whether any of this is universal.
Jeffreys is also a former student of Leon Kass, who is perhaps the most prominent advocate of appealing to disgust as the basis of his influential bioethical arguments against human cloning and stem cell research. However, other proponents of this approach have made similar appears to disgust in, for instance, discussions about the identification and definition of obscenity and employed similar lines of reasoning to argue against abortion, pornography, homosexuality. What most of these arguments seem to appeal to – either tacitly or otherwise – is a particular view of the nature of disgust itself as a morally attuned emotion into the “naturalness” (or, more importantly, “unnaturalness”) of certain activities and social practices.
Of course, the validity of Jeffreys appeals cannot be judged from the motives or affiliations of its champions. Judged solely on the merits of his arguments, how well does Jeffreys clarify the concept of disgust and make a case for it?
Not very well.
The Case for Responsible Disgust
Jeffreys acknowledges Martha Nussbaum’s (2004) criticism of the centrality of disgust and morality in matters where the stakes are high; given disgust’s spectacular appropriation by the political right throughout history, as a means of reinforcing the boundaries between self and “contaminating” Others that has fueled and perpetuated racism, anti-Semitism, homophobia, transphobia, and misogyny. Nevertheless, he firmly frames himself in opposition of Nussbaum (and encourages the reader to do the same – with no actual argument besides his opinion and what seems like an incomplete and/or mischaracterization of Nussbaum’s argument). In opposition to Nussbaum, who argues convincingly that disgust is inherent irrational and, thus, unlike the emotions of fear, compassion, and anger, disgust cannot be responsibly mobilized. Jeffreys disagrees with this argument – because his entire conceptual framework would otherwise fall apart. How? He simply tells the reader that the horrifying political times that Nussbaum refers to are a thing of the past. If you are a Nazi, you will agree with this argument. If you have been living under a rock and have no moral compass, you might agree. What makes it difficult to agree or disagree with Jeffreys is that he has strategically muddled up his entire argument on this topic at the level of syntax and with confusion over the concepts and under defined concepts such as “self-transcendence” that it’s difficult to really come to a strong opinion on his argument after only one reading. I found these chapters to be the most painful in the book – and that’s saying something.
Now that I have read this book more times than is healthy (which is more than once), I can lay out Jeffreys position and rhetorical moves a bit better. In answering the criticism of Nussbaum that disgust is a powerful weapon in the wrong hands, Jeffreys completely agrees but thinks that the risks of widespread violence and dehumanization against groups of marginalized and unpopular groups are well worth the potential individual benefits that disgust might bring “in prompting us to recall that we are bodily beings capable of self-transcendence” (p. 106). For example, Jeffreys writes, “when we recoil in disgust at learning of undocumented immigrants crowded in a jail cell without functioning toilets, disgust reminds us that such conditions are unfit for human beings” (p. 106).
First, I would like to know who “we” is supposed to be. I am not Jeffreys ideal audience. But even if we pretend that Jeffreys has made a convincing argument, that we are universally disgusted by non-functioning toilets and overcrowding in detention facilities, then why are these facilities not burdened to the ground? Well, that’s because Jeffreys doesn’t want you, the reader, to be grossed out by the idea that we are committing crimes against humanity. Instead, he wants you to be grossed out enough to demand that we build newer, bigger detection facilities, so every prisoner will be ensured a working toilet while they are stripped of their family and rights and, often times, their lives.
Let me move away from Jeffreys’ pseudo-humanism, Make America’s Jails Great Again moral monstrosity of a politic to demonstrate the his paltry intellectual offerings when it comes to the skill of deductive reasoning. For Jeffreys to even make an argument for responsible disgust as a window to self-transcendence – or whatever – means having to accept that responsible disgust can only be disgust with the effects of power, not weakness, among the marginalized. Given that Jeffreys stands aware and in agreement with Nussbaum’s critique of the political use of disgust becoming weaponized by political right for shameful and violent purposes. So, unless Jeffreys is just posturing here and actually tolerates racism, misogyny, anti-Semitism (and the like), he must insist on a concept of responsible disgust that is useful only for those with the least political power – such as prisoners and other groups who are unpopular and stigmatized by society (note: these are not cops or anyone in power today).
Not only is this unlikely given what can be deduced from the disturbing ideology of this text, it also doesn’t make much sense given that disgust does seem to play an important evolutionary role in alerting us to contamination and such. On all of this, Jeffreys has no satisfying answer.
Importantly, this moral condemnation of disgust does not yet prove, of course, that it is a major problem in the phenomenon of mass incarceration, let alone the central problem, or that it is a bigger problem than any other emotion like anger or fear. It shows, rather, that “disgust” is a moral category and therefore difficult to objectify in sociological research.
Conceptual Incoherence
The author’s treatment of the central concepts in his argument suffers from a lack of rigor, logic, precision, and clarity. These are only a few examples.
Insufficient Operational Definition
Jeffreys offers no sustained analysis of the operations of disgust and stigma that would help to convince the reader that these concepts would be ethically directed at protecting the dignity of jail inmates, rather than weaponized by those in power to maintain a culture of abuse and degradation against unpopular people or those who make the dominant majority uncomfortable.
Taking Inherent Dignity to it’s Logical Conclusion
Jeffreys employs a concept of inherent dignity that, as a philosophical ideal, is extended to all individual human beings, at all times, under all circumstances. This means that we, as people, are not merely things or objects or commodities. By possessing inherent human dignity, every person has a unique capacity for reason, autonomy, growth, and “self transcendence” in our inner lives. We all have a capacity for “goodness.”
For Jeffreys, jails are dehumanizing because they are deeply degrading places, turning prisoners from people into things. “Jails,” he writes, “are dehumanizing and degrading places where prisoners experience repeated assaults on their dignity. They often live in filthy and overcrowded conditions, are subjected to demeaning whole-body searches, and suffer violence and sexual assaults from inmates and jail staff…in captivity many inmates experience terrible despair, a sense of devaluation that leads them to engage in self-destructive behavior” (p. 7).
We also read that dehumanization results from stigmatization of current and former prisoners because their criminal status produces a “spoiled identity” that encourages other people to devalue their humanity and personhood. But we also read that there is nothing you can do as a person, including dehumanizing another person or 10,000 or even killing one (or 10,000) that can strip you of your dignity, especially if you seek redemption or self-transcendence through Christianity. This expansiveness is designed to render Jeffreys’ argument potentially unfalsifiable. Of course, his theory is a dud and we can see in practice whose dignity he chooses to center which is another indicator of the author’s deeply pernicious right-wing, evangelical, pseudo-progressive agenda. One more thing about logical fallacies and errors since there are going to be a lot of them upcoming. The burden of proof is squarely on Jeffreys to explain himself and make his argument jive in terms that are intellectual rigorous (Ha!) or at the very least, not based on lies, mythology, or wish-fulfillment. Disproving fallacies and errors is not a thing that anyone can do or has to do.
Lack of Clarity
Drawing inspiration from the work of Aurel Kolnai, Jeffreys holds that the provocation of revulsion also suggests its moral significance in the realm of human dignity: promoting “a different kind of encounter with others” (p. 85). Cool. What the hell does that mean?
“Vague appeals to social agreement cannot substitute for good ontological investigation” (p. 86). I am not sure what this means.
More Disgusting Stuff
Here’s some more repulsive content in this book.
Bizarre Sexual Obsession
Jeffreys combines overtly “disgusting” images of corporeal decay and sexual victimization. There is a bizarre fixation on sexual violence, child rape, and molestation in this book which animated by a notable Biblical homophobia, transphobia, sexism. Ironically, Jeffreys has nothing to say about the criminal pedophilia and disgust of the Catholic Church.
Homophobia
Does “disgust” apply to homosexuality? Jeffreys has a section on this, saying yes but answering no. “Debates about the morality of homosexuality, for example, often involve disgust responses. Despite our changing norms and attitudes (a positive development in my view) about homosexuality, some young men still respond disgust at the idea of men having sex with each other” (p. 107). In his view, homosexual sex acts often illicit a reflexive disgust that is God-given and natural. Jeffreys doesn’t tell us what he thinks about trans people.
Vehement Anti-Blackness:
“[W]e can identify general ways we denigrate dignity. A practice denigrates it when it treats a person merely as a thing, failing to recognize the shared and individual sources of dignity. This was Kant’s central insight, and it remains important even if we disagree with him on philosophical issues. Slavery and rape are paradigms of using others merely as objects for labor or sexual domination. They are not problematic just because they use people for personal benefit; such exchanges occur often in everyday life. Instead, they treat the person merely as a thing without recognizing his personhood. For example, when I got to the supermarket, the checkout clerk and I use each other. He provides me with a product, and my payment provides him with a job” (p. 92).
Fucking, eh. There is so much wrong here that it requires a list:
- Jeffreys decision to juxtapose “the paradigms” of slavery and rape speaks billions of volumes in a book that doesn’t even attempt to hide its white nationalism. That these practices are reprehensible not because they are literally slavery and rape but that objectifying in the same way that grocery shopping is when Jeffreys “uses” (rapes, enslaves) his checkout clerk and vice versa, who we can only assume is a Black man since Jeffreys has so kindly “provided him with a job” by purchasing a gallon of milk. What the fucking fuck? How else is this supposed to be read?
- It’s not clear if anyone who is not a white supremacist read this book, but certainly no one copy edited it. Consider the first and second sentences. The first is about the “general ways” that “we” – the reader – “denigrate dignity.” The next tells us that “[a] practice denigrates it when it treats a person merely as a thing.”
- It’s not clear why or how its relevant that this was presumably Kant’s central insight and deserves to be taken seriously “even if we disagree.” I assume because Kant is Kant. I don’t know anything about Kant other than he a Dead White Philosopher. It’s interesting that Jeffreys doesn’t even feature him in this book and still commands the reader to take his views seriously, while summarily dismissing the work of Angela Davis and other prominent Black women academics who he clearly has not read, but still references in his bibliography. Has Jeffreys read Kant? Who knows. My uninformed opinion is that Kant is probably garbage but also being misrepresented here.
I wish this example was an anomaly. It’s not. I also assure you that none of this is taken out of context. The book is a fucking mess.
Valuing Only Peaceful Racist Order
In Chapter 3, Jeffreys emphasizes a second understanding of dignity as a status granted to those who “show a gravitas in the face of injustice or suffering” (p. 73). This status is conferred specifically upon Black protests during the Civil Rights movement, in particular, he points out a 1963 protest in Jackson, Mississippi, where a mob of white supremacists surrounded a black student protestors at a lunch counter and assaulting them with physical violence. “Rather than respond violently, the protestors sat silently at the lunch counter. The Jackson protestors exhibited a dignity that we can all recognize as a remarkable response to adversity and injustice” (p. 73).
What does peaceful mean? Whose peace? What is the definition of violence? In anticipation that Jeffreys might come back with a reference to the civil disobedience of Dr. King, as a reminder, peaceful means and dialogue got him murdered.
No Comment
“When my disgust toward others becomes habitual, I no longer perceive value in all humanity. Affectively, I carve out an exception for members of a group (for example, jail inmates). Because they are disgusting, they no longer inhabit my circle of positive valuation. They are outliers, exceptions to a circle of care that can otherwise be quite broad. For example, I sometime meet people who consider themselves good liberals or progressives who respect human rights in many contexts. Yet when I mention inmates I have taught who have committed violent sexual assaults, our conversations come to a halt. They are visibly revolted, and evince no benevolence at all toward sex offenders of any kind. They see them as contaminated beings whom we need to quarantine and incapacitate” (p. 108).
Ew.
Final Comments
- His assessment of disgust depends on the use of criteria, which is related to moral values and social standards of normality. Jeffreys does not deal systematically with the question of what these criteria might entail. It is clear that what is “disgust” for some looks like “anger” or “pleasure” to others.
- It is by no means clear how being grossed out, even viscerally and strongly, by an act or situation plausibly leads to reforming – much less abolishing – that act or conditions of that situation. In fact, this argument feels constructed specifically as a way to gesture towards something progressive and moral with the intention of using it as a smoke screen for doing nothing.
- The capricious nature of emotions, that they can be highly erratic and based on arbitrary factors or ones that favor personal bias, would seem to be enough of a drawback to resist them as a foundational approach to moral decision making. How can we even determine what disgust is or whether it is felt consistently among everyone or the average person? What is the distinction between anger and disgust? To me, the feelings I have toward mass incarceration tend to incite emotions that (I think) feel more aligned and with anger than disgust. In particular, anger directed at the damage and harm caused by imprisonment. This feels much more productive than disgust. Anger has more liberatory possibility and hope, compared to disgust which feels flattened and stagnant.
- If people can be capable, they can be accountable.
Close Reading: Perspective and Representation
Method and Style
Unlocking the method and style of America’s Jails holds the key to understanding its double-nature and the type of reading it is asking of the reader.
Superficially speaking, that is to say the features on the surface of the book – as well as those contained within the introductory and concluding chapters – provide the most direct expression of the author’s aims and strategies. In America’s Jails, the relevant surface features are genre indicators, descriptive copy, epigraphs, and content from the introduction and conclusion.
Genre Confusion and Narrative Inconsistency
Most notably, the book – published by New York University Press – bears the subscriptions “criminology” and “alternative criminology” on its cover – two labels that lead to a vague notion that the text’s nature may not be all that it seems. As a category, “criminology” designates a genre where much consideration is given to the veracity of an account. Alternative Criminology is a special category that designates the publisher’s created book series. Currently edited by Jeff Ferrell, a sociologist at Texas Christian University and visiting criminologist at the University of Kent, the series:
is founded on an eclectic, cutting-edge sensibility that seeks to broaden mainstream criminological thinking” and “addresses and encourages the ongoing development of new criminological perspectives that challenge conventional understandings of crime, justice, and social control.
While such a buzzword-laden rebranding could, cynically or with some ire, be observed as a good way to sell more books, I think it’s fair to say that “alternative criminology” also reflects an earnest attempt to categorize the work of community of scholars sharing certain assumptions concerning society, crime, and punishment.
But calling America’s Jails an “alternative criminology” text is problematic because it’s untrue.
While the Jeffreys may have pitched his book as an “alternative” to mainstream criminological and social scientific approaches to crime and punishment, the book fails to offer anything that might be considered as provocative or new. Jeffreys’ does not “challenge conventional understandings of crime, justice, and social control.” On the contrary, he reifies and reinforces them. Ironically, that this book was published by a non-profit university press where social justice branding is nearly universal demonstrates the “cutting-edge sensibility” of Jeffreys’ project.
America’s Jails is old wine in new bottles; a fake thing pretending to be real. A non-alternative alternative that perpetuates a culture of punishment. We know this because the author’s views and perspective on crime, justice, and social control are exactly the same as the State, and since the State doesn’t identify as “alternative” or “radical,” then Jeffreys isn’t alternative or radical either. It’s really as simple as that.
But more complicated, is this book’s official genre category of . “criminology” given that Jeffreys has made it more than clear vehemently that his project is in-no-way-shape-or-form methodologically criminological or sociological. Throughout the book, Jeffreys presents his project as a much-needed critique of criminology and sociology that he accuses of having too often ignored history, neglected the lived experiences of prisoners, and confused rhetoric for reality. In his conclusion, Jeffreys’ stance becomes even more direct when he writes:
“[A]s established fields, criminology and sociology fail in their attempts to “overcome the evils” that plague the criminal justice system by treating crime as a technical matter, rather than a moral one” (p. 165).
The debate becomes game, set, match in the first several pages of the introduction, where Jeffreys, not known for his clarity or directness, tells the reader – twice – that he is NOT a criminologist (nor does he appear to play one on TV):
- “I am neither a sociologist nor a criminologist, and will therefore offer no original social-scientific research in this book. I am a professor religion and philosophy who believes it’s important to engage with social-scientific and historical approaches to punishment” (p. 3).
- “Because I am not a criminologist, I don’t follow all the debates about reform and abolition, but I have learned a great deal from them” (p. 11). (This is a remarkable statement given that: (a) it doesn’t make any sense; and (b) Jeffreys devotes 30-40% of the book to the “reform vs. abolition” debate).
(Emphasis added)
So, what can we make of a book that claims – all at once – to be criminology, alternative criminology, and not-at-all criminology?
According to Jeffreys, America’s Jails is philosophical and anchored in the “early phenomenological tradition” of Husserl and other Dead European White Men. I don’t know much about phemenology, but Jeffreys is talking about pre-Heidegger phenomenology. In the final pages, he reiterates his method, writing:
“In this book, I have added the philosophically sophisticated perspective of phenomenology to contemporary discussions of the jail” (p. 175).
To me, this raises alarm bells and indicates there’s definitely something disturbing and elusive brewing in this book. Calling an 18th century phenomenology indebted to 1920s psychoanalysis a “radical” and “edgy” seems more than a little problematic? After all, it is 2019. Granted, I don’t speak with expertise on phenomenology, but something doesn’t sound right.
For one thing, I did not read this book as phenomenology; I think it is more a religiousy autobiographical novel (a confessional memoir?), and I do not mean that as an indictment of phenomenology, to which I would not apply that label in general.
I am more than confident that this book’s best genre clue rests in the epigraphs preceding the introduction and conclusion chapters. Epigraphs are often short quotations that serve to link a text to other well-known, published works. In Rewriting: How to Do Things with Texts, Joseph Harris describes epigraphs as commenting on the text that follows by setting tone and suggesting a perspective. “When done well,” he argues, “an epigraph can serve as a kind of poetic précis of a text, summing up its main scope – even if its full meaning does not always become clear until the piece has been read through and epigraph considered a second time” (2006, pp. 30–31).
In America’s Jails, these symbolic passages come from Fyodor Dostoevsky’s semi-autobiographical novel, House of the Dead. In this story, the reader experiences prison life from the perspective of Alexander Petrovich Goryanchikov who been sentenced to a decade in prison for murdering his wife in an act of domestic violence (a sentence that was remarkably mitigated due to his confession of the crime). As a newcomer and a “gentleman,” life in prison is terrible for Goryanchikov, who writes of the squalid living conditions, the packed crowds of “living dead.” He experiences repulsion at his circumstances. However, gradually over time his views on prison life – namely, prisoners – change as he takes note of their humanity, and eventually he undergoes a spiritual transformation that culminates in his release from prison.
The introductory epigraph represents a symbolic passage at a key moment in the book where the narrator experiences a spiritual re-awakening that enables him to finally “see the light.” Across four dense sentences, Goryanchikov experinces an epiphany about prison life and human nature, “discovering” that “real life” is just too messy, cluttered, and multifarious to allow for the classification and abstracting of prisoners, of people. He finally realizes that what a person calls their own life – that is, their “inner life” – is too stubbornly entrenched to bend to outside pressures and control:
“But I have been trying to classify all prisoners and that is hardly possible. Real life is infinite in its varieties in comparison with even the cleverest abstract generalization and it does not admit of sweeping distinctions. The tendency of real life is always toward greater and greater differentiation. We, too, had a life of our own sort and it was not a mere official existence but an inner life of its own.”
The final epigraph is a bit more mysterious, but seems to be suggesting to me Jeffreys’ emphasis on public safety for accepting prisons as a tragic fact of life. Here, the rhetoric of danger is prominent as Dostoevsky writes about a “criminal” made more dangerous by their imprisonment.
“Of course, prisons and penal servitude do not reform the criminal; they only punish him and protect society from further attacks on its security. In the criminal, prison and the severest hard labor only develop hatred, lust for forbidden pleasures and a fearful levity.”
By all accounts, House of the Dead is the canonical parallel of America’s Jails – in the sense that Jeffreys has obviously used this book as his template for constructing his book. The similarities are too striking to be coincidental when you consider that House of the Dead is: (a) famous for its uncertainties regarding genre, subtly lingering between fiction, philosophical musings, documentary, and memoir; (b) characterized a distinctly detached, “objective” hero-narrator who stands back, focusing more on categorizing the personalities and events of the other prisoners, but who, from time to time, allows his introspective voice to come through; and (c) presented more as a personal diary or a series of vignettes experienced by the author, pulled together by a common “theme”; (d) a book with deep religious undertones. These are only a few of the similarties.
Jeffreys has essentially used the ficitional account of Russian prison life in House of the Dead as a blueprint for his entire book. A non-fiction “criminology” book. The use of this book as a template raises major questions about the veracity of this account, as well as the author’s trustworthiness and credibility. America’s Jails also belongs to a class of books that straddles the border between fact and fiction. As I see it, America’s Jails is a wannabe Dostoeviskian portrayal of the contemporary jail system from the not-so-Dostoeviskian perspective of outsider. It’s a shallow and egergiously unethical attempt to mirror its tone, themes, structure, and, most importantly, it’s ambiguous genre – presenting itself as a nonfiction scholarly anti-prison polemic while modeling the exact same delusive fictional shell for the presentation of Jeffreys own observations and true-to-life memories of the US jail system.
House of the Dead is a work of prison literature – straddling uneasily the borders between fictional novel and autobiographical memoir. The book presents an authentic account of prison life in Russia, narrated from the perspective of a fictiona prisoner-person. The authenticity of the account comes from Dostoevsky’s personal experience and authority to speak on matters related to incarceration. As a political prisoner in a Siberian work camp, Dostoevsky’s perspective allows him to write about an insider on the inside from the perspective of an insider.
America’s Jails is also advertised as a book written about insiders on the insider from the perspective of insiders. The descriptions on the back cover were the reason I chose to read this book. I expected this book to tell the story of jail from the perspective of prisoners. Consider the two paragraphs of descriptive copy, each seems to be indicating that this book will be a prisoner-victim-centered discourse:
- “In America’s Jails, Derek Jeffreys draws on sociology, philosophy, history, and his personal experience as a volunteer in jails and prisons to reach a full understanding of the jail experience from the inmates perspective, focusing on the stigma that surrounds incarceration.”
- “Highlighting the experiences of inmates themselves, America’s Jails aims to shift public perception and understanding of jail inmates to center their inherent dignity and help eliminate the stigma attached to their incarceration.”
(Emphasis added).
This is all a lie. America’s Jails only claims to be an insider on the inside account of the essential of jail experience from the perspective of insiders. In reality, this book is written from the perspective of an outsider on the insider (in the most superficial way) presenting an understanding of the day-to-day reality of jail experience of insiders from his perspective. Whether this is false advertising or self-sabotage, the result makes for an exasperating read.
This is one lie of many, but it’s a significant one. The absence of prisoner voices in this book illustrates one of the biggest problems found in modern stories of mass incarceration as the issue is not only what is being said but who is speaking as well. Given the history of privileged white outsiders claiming the “truth” or marginalized lives better than marginalized people themselves—and the exercises of power which such claims have enabled—the author’s choice to center himself is absolutely reprehensible.
In America’s Jails, Jeffreys shapes an experience of jail that begins with himself and is much more in service of the experience than it is to external facts and context. With this perspective, the jail is constantly mystified and mythologized. It is against this backdrop that I argue that America’s Jails ritualizes a violent order, rather than disturb or disrupt it. This book is a pro-prison discourse because it others prisoners by presenting them in sharp contrast to “exceptional” heroes – the author as well as police and prison staff.
Visual criminologist Michelle Brown (2009) uses the notion of “penal spectator” to describe the individual and institutional means of looking at other’s people’s pain from a distance and perpetuating ideologies and indexing logics of punishment in the process. As such, penal spectatorship allows the spectator to witness and consume the pain of others, without direct participation in the visceral realities of crime, victimization, and punishment. Brown refers to the penal spectator as someone who “looks in on punishment and yet is also the author.” This means that the author is in control of the punishment they are looking at. As such, they can create their own reality.
For Jeffreys, (what is taken to be) “reality” relies solely upon an ersatz interior account of the conditions of jails and the prisoners within them from viewpoint of the author. Bizarrely, prisoners’ experiences, their views, feelings, fears, and yearnings are omitted. Their knowledge, subjugated and marginalized, would have provided an alternative truth to the authors’ dissembling definition of penal reality. None are quoted, and in the cases where they are described, they usually serve either to repeat his conclusions back to him or to serve as a negative object.
Jeffreys uses a form of penal spectatorship that is rooted in the first-person, subjective exploration of jail and self. Despite its promise to focus center the lived experience of prisoners, this book focuses on the author’s self-transformation – and not prisoners. The reader experiences the day-to-day reality inside US jails from the perspective of Jeffreys who purports to be modeling the experiences of prisoners. Jail, as experienced from the author’s pathos-filled perspective, involves voyeuristic suffering, egregious appropriation of prisoners’ voices, and silent apathy toward the real violence directed at the vulnerable. This method relies solely on the author’s personal experience and his self-transformation. The result is the rhetorical erasure of the victims.3
Prison Voyeurism
This form of prison spectatorship is also referred to as prison voyeurism which “attempts to understand and/or experience corrections without intimately engaging in the subject matter” and is often “characterized in terms of economic, physical, mental, emotional, and psychological investment in an experience” (Ross 2015, p. 400). Basically, prison voyeurism as an approach reflects both a failure to meaningfully engage with the subject material and a possible means by which an author can gesture towards a meaningful, substantive exploration of incarceration while actually using prison in a shallow way that enables the author to center themselves.
Prison voyeurism reproduces myths and misconceptions about mass incarceration that frustrate society’s abilities to reform. This is because, as an approach, prison voyeurism is defined by the following:
- Author’s outside on inside perspective
- Reader shares the author’s perspective
- Perpetuates voyeuristic perspective
In America’s Jails, Jeffreys employs this notion of penal voyeurism through the form of a jail tour, where the author, a white male professor of religion and philosophy, privileges his own emotional experiences to “describe some of the conditions that inmate experience” (p. 16). This is a method that constantly mystifies and mythologizes jail. The substance of the author’s experience in this book, as it were, comes primarily from two private tours of Cook County Jail in Chicago, Illinois, in 2013 and 2014, as an “authorized visitor” (p. 15) of Sheriff Tom Dart. From this point of view – the warden’s special guest – Jeffreys shapes an experience of jail that begins with himself and is much more in service of the experience than it is to external facts, providing readers “with a snapshot” (p. 24) of what he witnessed. Jeffreys’ privileged status and mobility enabled him to “stumble,” by chance, in and out of events4, which he reports in meticulous detail for the reader as representative of jail, as it really is. While this research approach might be intriguing to some, prison tours as a method are morally and intellectually useless: at best they are non-informative, usually a charade. At worse they co-opt or enable the visitor into a dehumanizing spectacle.
The prison tour, even as it brings visitors into contact with the original architecture and machinery of the penitentiary, acts carefully to distance us as outsiders in its privileging of cultural associations and stereotypical images of criminals over a more thoughtful structure, which links history with the unprecedented contemporary dimensions and sociology of imprisonment. (Brown 2009, p. 113).
Jeffreys method of prison spectatorship/prison voyeurism reinforces stereotypes pernicious stereotypes about prisoners and prison staff, and therefore, happens our ability to move beyond punitive mentalities. As a spectator to a sensational, and seductive, spectacle of disgust, Jeffreys invites his readers to celebrate the easeful and ever dangerous commingling of the prison and self. Jeffreys uses prisoners as philosophical “tools” meant to re-center the humanity of himself and other heroes – police and prison personnel. In this book, prisoners aren’t people; they are tropes, caricatures, and anecdotes to spice up a privileged “intellectual” discourse. If person’s life is only valuable insofar as those in power can be separated from their bodies to highlight someone else’s experience while the same incarcerated people remain degraded, then this “value” is actually violence.
Centering Exceptions
Despite claiming to center the dignity of the incarcerated, it only takes Jeffreys six pages into the introduction to shoot himself in the foot and betray his proffered cause. This book is framed against against mythical mainstream representations of jail that he claims reinforce a greater societal tendency to demonize police and prison guards by frequently portraying “sadistic wardens and malevolent correctional officers” in the popular media, which appeal to a fearful public seeking “a villain they claim blame.” He writes:
“Undoubtedly, the U.S. penal system contains no shortage of abusive personnel: corrupt judges, power-hungry sheriffs, pandering prosecutors, and violent and abusive corrections officers. However, I resist the temptation to demonize those working in corrections. Corrections officers have a very difficult job, and on a daily basis deal with troubled and violent people. I have met many corrections personnel who struggle to make positive changes in a broken criminal justice system. In this book, I feature people who accomplish remarkable things in horrible circumstances.”
(Emphasis added).
Now, there are several things to say about this, but let’s start with claim itself: Jeffreys’ point is so sharp that it becomes narrow, and there’s a begged question that holds together everything as follows: What popular television shows and movies has he been watching of late?
Not only is this a non sequitur, with the typical tortured use of “many” to avoid empirically anchoring an anecdote, it’s also morally repugnant nonsense. Mainstream media depictions of cops is exactly the opposite of what Jeffreys is claiming here. They are most often portrayed as fair and just in every situation, that every criminal deserves what they get.
It would be nice for Jeffreys to provide an example of what he is referring to but, as will become clear throughout this long post, Jeffreys speaks in abstracts and categories – never individual examples or citations. It is safe to say that the reason he does not give us any more information about these hypothetical demonizing tv shows about jails is because they do not exist. But if they do, I’d would love to know what they are. I’ll wait…
In the meantime, the truth is that the media routinely present police and prison officials as heroes. Noble, risk-taking, selfless, altruistic, who sacrifice themselves for the good of the community and are constantly put in harms way by evil or crazy criminals. As for the widespread demonization of cops by the US public? A Gallup poll in late 2017 found that 56 percent of Americans rate the honesty and ethical standards of cops as high or very high, an approval rating comparable to high school teachers and dentists – hardly your typical villains. Only 12 percent of respondents had low or very low opinions of police honesty. And this is not a reflection, for the most part, of people’s actual interactions with police. It’s the reflection of how television dramas and local news specifically portray cops.
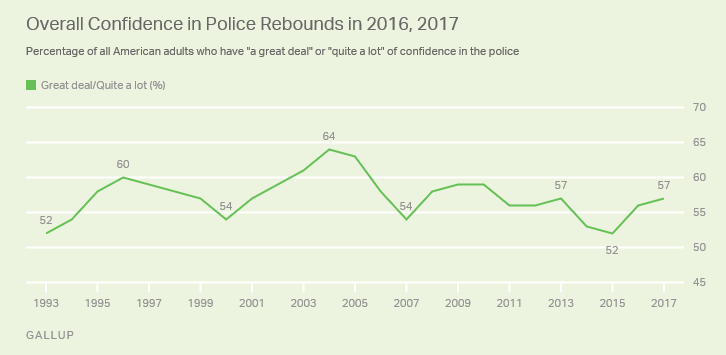
Copaganda
This book provides a useful study of how the carceral architecture of white supremacy is expanding right now via bipartisan criminal justice reform.
What Jeffreys is parroting here is a form of “blue racism” propagandist garbage invented by police departments that seek to turn around criticisms of racism against the police by claiming that it’s actually the police who are victims of racism: it treats “blue” as a race, arguing that a police badge and uniform colors is how typical Americans see a person, with negative results. Its objectively false, white nationalist garbage. And I’m certain that’s the premise upon which this book sits. America’s Jails meets all the criteria for being “copaganda” – a term generally used to describe puff pieces, typically fed to the local news by the police himself, that’s designed to burnish the perception and reputation of the police. There will be A LOT more evidence for this claim shortly.
In any case, returning to the above passage, it just so happens that everything you need to know about what makes Jeffreys such a compelling and reasonable sounding intellectual is right there. The elements that define this passage have evolved by now into a unique and inimitable style, one well-suited to an “post-racial” era seeking a parsimonious, condensed, and comfortable, and even, feel-good account of societal carcerality. In this way, this book almost immediately identifies itself as a hit among a wider (and whiter) audience who want to learn something about a topic in a way that does not demand rigor or any emotional downsides and is entertaining, and even fun, to “understand.”
From my perspective, the most fundamental problem with the book stems from the author’s overwhelming and questioned sympathy and defense of police and prison guards who, beyond Jeffreys’ personal opinions, have not remotely earned or even ethically warranted such praise or benefit of the doubt. This a pedestal that we are better off leaving empty. Jeffreys doesn’t just praise them, though. He romanticizes them to a degree that sets off alarm bells regarding his personal involvement with his prison and police sources (whose opinions on prison violence and jail life are presented uncritically as truth even though its objectively established that cops lie all the time) and political motivations for writing this book. Again, if this book were merely another popular right-wing, evangelical text on “prison reform,” it wouldn’t be worth getting worked up about. But this book presents itself as a respectable scholarly text by an author who has apparently done a good enough job of hiding its lack of rigor and lack of morals that I find it worthwhile to analyze just how much this book fails to be what it claims to be.
Of course, because you can only spin the truth so far, Jeffreys is unable to dismiss the existence of bad cops too. After all, he understands that violence against prisoners is morally inexcusable and that it is overwhelmingly committed by cops. But he also wants the reader to believe that these are rogue cops, not all of them, and by creating a caesura between the abusive state – “corrupt judges, power-hungry sheriffs, pandering prosecutors, and violent and abusive correctional officers” (p. 6) – and “hardworking and dedicated” prison staff, he can make his argument seem reasonable and convincing even when it’s objectively false. By abstracting the thousands of people who are killed by police or die in jail each year, reducing statistics to “systematic violence and neglect,” Jeffreys can plug in a straw man that assumes “both sides” share equal culpability and power which has never been true. This tactic may come dressed in a veneer of concern and moral parity but it’s nothing more than a performative way to pathologize criminality and victim-blame. This is all at odds with the unkept promises of this book. Demanding that abusers and oppressors be coddled, without contrition or change, isn’t morality. It is also oppression.
Such an approach epitomizes a phenomenon described by Teju Cole as “The White Savior Industrial Complex,” which, he writes, “is about having a big emotional experience that validates privilege.” Through each brush with danger and encounter with the oppressed, Jeffreys earns his otherwise cushy and free lifestyle.
It bears mention that the people who Jeffreys almost chooses to help are young mothers. In one interaction that is remarkable, for both its deviation from his usual stories and for its incredulity, Jeffreys paints himself as a hero who has his hands tied. When I first read it, I couldn’t even contain my incredulity, writing in the margins: “This NEVER happened. Fake News.” Let me be clear: I’m not suggesting that Jeffreys fabricated all of the accounts in this book. On the other hand, I’m not not saying that the following account isn’t 1000% completely fabulist fanfic. Both sides, you see. Since the passage is long, I will only quote the most relevant parts. However, the context for this scene is also noteworthy in ways that I will hopefully elucidate later with other examples. In this word-image, Jeffreys is narrating his tour of Cook County Jail’s new Residential Treatment Unit (RTU), specifically a dormitory for prisoners with mental illness. He begins his description by observing a room full of video visitation screens that have been implemented to replace face-to-face visits, a measure that he cannot seem to comprehend despite the fact that this is by now an established trend throughout the US jail system for a while now. In this scene, Jeffreys is just about to approach a jail guard for more information on this switch-a-roo, when he is suddenly interrupted. Jeffreys writes:
“I was approached by several women begging me and my guide to return them to a part of the facility where they could see their children. I, of course, could say nothing, but my guide told these women that there was nothing that could be done. They had been determined to have mental illness, and must remain in the new unit. One woman angrily denied that she was mentally ill, and became so upset that we had to retreat from her. Although I understood the need to save money, I couldn’t fathom how the jail could help people recover from mental illness by denying them close contact with family” (p. 32).
Of note, the passage ends with a rare citation in the form of a footnote, which, when followed brings the reader to the following entry:
“Human Rights Watch (2015). This report provides numerous examples of staff violence against inmates with mental illness in jails and prisons” (p. 186).
The massive report that Jeffreys is referring is based on a yearlong study of neglect by prison staff against prisoners with mental illness in the nation’s 5,100. “Callous and Cruel: Use of Force Against Inmates with Disabilities in U.S. Jails and Prisons. It’s a very harrowing and important report that was produced to account for the horrific neglect and violence that prison staff have inflicted upon prisoners suffering from mental illness, including assaulting them with chemical sprays, shocking them with powerful stun guns, and strapping them for days in restraining chairs and beds. The report contains This numerous accounts of staff who have broken prisoners’ jaws, noses, ribs; left them with lacerations requiring stitches, second-degree burns, and damaged organs. In some cases, this force has led to their death as was the case with Jerome Laudman, an intellectually disabled prisoner who suffered from schizophrenia, who, while being transferred to a supermax facility was severely beaten by prison guards (despite reports that he was neither combative nor threatening), who sprayed him with chemical agents. Upon his arrival at the new prison, he was stripped naked and put in a cold, bare concrete cell, where he was left for days until a guard noticed that he didn’t look so good and decided to transfer him to a hospital where he was diagnosed with hypothermia and later died of a heart attack.
For Jeffreys to make a statement, not only a claim, but accusation of assault against a nameless woman with mental illness and then footnote it with a report that documents the widespread and systematic neglect of people with mental illnesses in jails is appalling. And it tells you everything you need to know about how Jeffreys can produce a moral reprehensible book with just enough careful touches and elements of truth that it can pass as reasonable and compelling sounding from a scholar who appears to have thought carefully about what he’s doing. He sure has, but the image of Jeffreys as a reasonable and rigorous scholar is far from accurate.
There are other issues here, obvious, with the cost-saving part which Jeffreys seems to completely accept as valid, demonstrating either his “fiscally sociopath conservative” political leanings or his in ability to critically engage in anything. (Lastly, there is the weird phrasing of “they were determined to have mental illness” – who says that?).
The white savior complex is on display in one more example that borders on parody in the sense that it defies belief. In the following passage, Jeffreys narrates the absolutely embarrassingly implausible “event” of walking into a jail with as a white dude with a cop and being immediately approached by a hoard of prisoners, begging him to post their bail and regaling him with impromptu confessions about nature of the crimes for which they are “legally innocent” (according to Jeffreys) and still awaiting trial. He writes:
“When I entered a male dormitory one afternoon, numerous inmates suddenly surrounded me. Some thought I was a lawyer, and begged me to intervene to help them post bail. They were disappointed when they learned that I was a professor who couldn’t offer them legal aid. Others told me sad stories of being arrested for minor property theft or inappropriate public behavior. Initially, some inmates seemed rational, but then told strange and incoherent stories” (p. 30).
This farcical vignette is so audacious and vulgar that it defies comprehension. It simply has no basis in reality. Again, I can’t say that this absolutely did not occur, but I will say that this did not occur in reality. Moreover, the fact that Jeffreys the fact that Jeffreys needs to construct such embarrassingly silly narratives “events” in order to center himself with a halo before a flock of sinners is something that should be worked out with a professional therapist, at the very least.
The value-judgements dripping in these “reports” passes the point of parody. Did anyone insist upon verification or support for these claims. Did anyone during the peer review process at New York University Press that I’m not allowed to know about suggest anything here? Did these “events” actually occur and were they addressed by editor?
[Narrator: “They didn’t and they weren’t”]
Rhetorical Style
America’s Jails is less interesting for its anecdotes and arguments than as an epitome of contemporary rhetorical style that wants above all to be civil and reasonable. With the accoutrements of logical thinking and endless adverbs, Jeffreys can actively set the conditions for a more gauzy and comfortable conversation about mass incarceration is rooted in conflict avoidance and denial and serves to establish a power-serving tautology that centers the humanity of an unthreatened majority at the expense of its vulnerable victims. By always teetering around the margins of acceptable opinion, Jeffreys finds safety in the middle. What we get is a whitewashed, unsourced, and revisionist narrative.
It is not just that this book represents yet another conventional story of mass incarceration by an outsider authority who has appointed him a relevant arbitrator on matters he is only tenuously familiar with but that Jeffreys has actually written a reasonable (enough) sounding and compelling book that contains enough rhetorical moves to disguise its conservative and religious agenda. In fact, it’s a book that doesn’t really seem to have politics. At least not on its surface. This set-up makes the author’s proposed conservative right-wing policies seem “reasonable” in the short run, while ensuring the prison industrial complex is entrenched with new avenues for profiteering.
At the same time, Jeffreys employs rhetorical tics and modes of prose that portray him as an “objective” and detached observer – giving an aire of reasonableness and authoritative authorship to the text. But this view of Jeffreys as a reasonable and conscientious scholar is far from accurate. Rather than handle the sensationalism of its material with great care and insight; this book promotes the narcissism of the privileged white gaze – a gaze that often has a cis male heterosexual structure – to an unconscionable degree.
He accomplishes a lot by remaning super vague and speaking in platitudes to avoid being called out and forced to reveal his odious political motivations. With all the accoutrements of logical thinking and a barrage of adverbs, Jeffreys can actively set the conditions for a more gauzy and fun conversation about mass incarceration. It’s an example of what Tayari Jones calls “the ‘both sides are good phenomenon’ phenomenon, an approach rooted rooted in conflict avoidance and denial.” This allows Jeffreys to live a Manichaean world where he can easily lament “the degrading character of the arrest process in the case of Chicago policing, which has often exhibited racism and violence towards those arrested,” but in the next sentence write, “The Chicago Police Department is an enormous institution with many fine employees who treat people well” (p. 133). Throughout the book, Jeffreys presents himself as an author unduly production of his own magnanimity in admitting that he will not hold anyone accountable for abuse or violence. However, such elaborate syntactical balancing evens out at meaningless. What Jeffreys’ refuses to see is that there are no “both sides have a point” when one side is dehumanization and other is survival. There are material fucking consequences for people’s lives and this faux-intellectualism has no place in a book about mass incarceration.
Reasonableness and civility are just ploys that allow one to just amble along, shouting things like “All Lives Matter” and “shut up with your protests and violent protests” and “let’s just get to dignified politics” where everything is just a matter of opinion, “agree to disagree,” and nothing actually changes ever and you know exactly the same shit will happen again and again and again because no one is challenging anything in any case.
Language
An important support for the portrayals in this book is language.
Use of Stigmatizing Terms
Jeffreys refers to prisoners and marginalized as: inmates, criminals, jail targets (militaristic), undocumented. They are never referred as victims.By contrast, captors are accorded respect with titles: correctional/jail officers (as opposed to guards, captors, criminals, abusers). Behind such language is a pervasive double standard in how we often think about crime.
Representations of “People” in Prison
Right-wing populists like Jeffreys often present themselves as siding with the “people” against the opposition (enemy). Importantly, “the people” represented by the author is ill-defined for strategic reasons, allowing him to call a particular “people” into being.
“Other people find convenient excuses or rationalizations to ignore violations of inherent dignity. They claim to know little about the jails in their community. Or they assume that all inmates are liars who fabricate stories about jail violence. Finally, they may harbor strong views about American exceptionalism that blind them to the brutality of our jails. For many Americans, terrible violence in jails simply doesn’t happen in their country; it occurs only in unjust regimes in other countries. Such thinking enables them to turn away from obvious assaults on dignity in their local jails” (p. 94).
A Specifically White “We”
- “We are also learning more about the racial discrimination that pervades our criminal justice system” (p.155).
Jeffreys and I do not fight for the same thing. There is no “us.” There is Them and any attempt to minimize state violence makes you an enemy.
Important point: the opposition (enemy) crafted throughout this book’s discourse style is not simply targeting the author, but also “the people” represented by the author. Yet, much like the vague and shadowy enemy looming in the midst, “the people” is ill-defined for strategic reasons and allows the author the ability to call a particular “people” into being. In this case, “other people” is the author himself.
Metaphors
He uses the metaphor of assault – both in his first person accounts of jail experience, as well as in his philosophical discussion of dignity and disgust. The use of the metaphor in both types of writing indicates that Jeffreys considers himself a “victim” of the degrading conditions of jail. This particular metaphor is explicit and forceful given that he intentionally hides away the actual, real violence that occurs against vulnerable prisoners – the real life victims.
- “We entered a maze of tunnels, and I immediately experienced sensory assault” (p. 15).
- “Horrible sanitary conditions in jails assault inherent dignity by stifling a person’s capacity to express self-transcendence” (p. 94).
Moral Use of Marginalized
Jeffreys writes early in the book of his decision to use “marginalized” as a word to “refer to those whom the jail targets” (p. 5). While this seems like a progressive move, it’s not quite the one it’s claimed to be. This is because it is not concerned with individual liberation, social equality, and social justice. In fact, as Jeffreys describes it: “I use it in a moral and nonmoral sense to include a variety of people. It can refer to those who commit terrible crimes and evil acts that endanger others. Or it can denote those whom a community finds (with or without good reason) problematic, different, risky, or annoying” (p. 5). In other words, marginalized is operationalized in a way that makes it morally useless since it can be applied to anyone. It’s important to note that in the decision to use “marginalized” was based on the suggestion anonymous reviewer during the peer review process at NYU press who suggested that it replace his earlier term, “deviant” which Jeffreys wants to assure us was intended in an entirely sociological and nonmoral sense (p. 181). The problem with Jeffreys’ earlier desire to use the controversial term “deviant” in a nonmoral sense minimizes the fact that the term represents more than the sum of its parts. There is a deep embedded meaning in the term and the word represents much more than its intended sociological usage.
Devilish Details
Hardly Evidence
To make such an extreme claim in a book published by a leading university press, surely one must have some pretty damning evidence? Nah. Gut feelings and opinions are fine.
- “I have met many corrections personnel who struggle to make positive changes in a broken criminal justice system” (p. 6).
- “Not all U.S. jails are mismanaged hellholes. Some compassionate sheriffs and staff work hard to prevent violence and maintain minimally decent health care and sanitation” (p. 66).
- “I have a friend who works in a jail that negotiated a DOJ Consent Decree. Monitors conduct regular inspections, and the jail has seen some important improvements. Jail conditions remain imperfect, and problems at the facility persist. However, my friend welcomes the DOJ’s presence, likening it to parents keeping an eye on their children. He believes that such a watchful eye is a positive development, and hopes that the DOJ will bring enduring changes” (p. 134).
- “In my years teaching in prisons and jails, I have spent a lot of time talking to corrections officers. Sometimes I meet veteran officers who work hard to respect the dignity of inmates…They give orders and expect inmates to follow them, yet speak respectfully to them. They also strive to treat inmates fairly” (p. 152). (The final pages of the conclusion end with four paragraphs devoted to veteran prison guards who have informed this entire theory).
How Jeffreys’ personal experience or opinions from his friends are worth anything of value in this conversation is beyond me. Your fucking opinions are not evidence. And yet…such unsupportable generalizations billow on and on in this book.
It should be obvious that an explanation of institutional change that hangs on the official claims of prison personnel themselves is clearly inadequate, even if – and this is a crucial caveat – those prison personnel are honestly conveying what they think they are doing and why.
Who are these people and what are these positive changes? I, for one, would like to see this evidence. Who are these people and what are these positive changes? What are some examples of non-hellish jails? Please cite one example of the “jail officials [who]rarely abandon inmates…but instead treat them humanely” (p. 44). I’ll wait…
Reparative Reading
Sloppy Treatment of Mental Illness
Jeffreys slapdash analysis of mental illness is probably the most irritating component of this book. Again, I am angry because I care about this topic. My jail experience is directly related to a diagnosis of schizophrenia. While my experience is only my own and doesn’t remotely speak to the violence and neglect suffered by others, I have seen first-hand how often prison staff neglect the severely mentally ill by not only refusing them medication (which has been my experience and the experience of many people I have talked to, which is in stark contrast to Jeffreys claim that psychiatric staff are hampered the procedural red tape involved in obtaining legal authority to forcibly medicating prisoners in severe mental distress; something Jeffreys absolutely believes is unfair to prison staff as it can “involve a hearing that takes a day or longer, and requires staff members to go to court” (p. 29). I spent months in a state hospital only to come back to a jail and be refused my court-ordered medication for several days. In fact, I never received it because I was bonded out. I later found out all along that the jail had the prescription but refused to give me my medications. I would also like to point out that I had a great attorney working on my behalf, as well as outside advocates, and my mental health was still neglected. Which is why it absolutely enrages me to see Jeffreys recasts jailers as caring social service providers, going so far as to “marvel” at the “commitment” of “a dedicated young psychiatrist” who managed to doing no more than “work with patients all day” – his literal chosen profession for which he is paid (p. 29). Again, if these statements provoke or unsettle the reader that’s because Jeffreys is lying. But I will admit that, on their own, these are rather uninteresting. They function in their totality to tell a disgusting fabulist account of US jails that is odious.
“Mental health care areas can be dangerous places for inmates and staff” (p. 30).
This is only ever meaningful when its also followed up with facts about how people with mental illness are much more likely to be victims than perpetrators of violence. Individuals diagnosed with schizophrenia, one of the most stigmatized mental illnesses in terms of fear of violence, are victimized by police at rates 65 to 130 percent more frequently according to police incident reports (Metzl and MacLeish 2015). Jeffreys follows this statement up with a paragraph devoted to a sensationalist media story where a mentally ill inmate murdered other inmates. He offers no vignettes or case studies of violence against mentally ill prisoners by prison staff. Rather, he presents two more extreme examples of people with schizophrenia who gouged their eyes out while in custody. Of the other news stories, Jeffreys features prisoners who engage in self-harm or suicide.
Marvelling
“A psychologist I met worked hard to help inmates” (p. 31) – This is presented without any explanation or further information about how or what this even means. And we are just supposed to believe this statement. And that’s a tough thing to do given that the vast majority of drug dealers have better ethics than Jeffreys.
“I met a dedicated young psychiatrist who worked with acute care patients. I admired his commitment and marveled at how he could work with patients all day” (p. 29).
“Dedicated but overwhelmed health staff struggle to help these inmates in some minimal way. Overall, custodial and therapeutic goals seemed to coexist awkwardly at the Cook County Jail” (p. 31).
I spoke with the social workers doing them [intake mental health interviews] and expressed admiration for the difficult job they were performing” (p. 25-26).
In another example, Jeffreys claims that if Cook County Jail is neglectful towards the mentally ill, its because they cannot find qualified mental health staff since “correctional mental health is an extremely difficult job” (p. 32). How so? He doesn’t say. He wants to present this as obvious but such statements require explanation and evidence. It is not remotely clear how correctional mental healthcare is. more difficult than working in an overcrowded, state run clinic or hospital? If it actually is more dangerous (as Jeffreys surely believes it to be), it is certainly because abusive staff, coercive punitive culture of prison is making it that way.
I have much more to say about Jeffreys’ awful treatment of mental health in this book, but I am tried of re-inventing the wheel so I am copying and pasting from some of my earlier reading notes. In particular, here are two other ways (again, of many) that Jeffreys betrays is an appalling level of ineptitude for talking with any any degree of authority on a topic where the stakes are so high:
Jeffreys uncritically deals with the calls for opening up state hospitals again by suggesting that they would be the same as they were in the 20th century with same horrors. He argues that “this narrative suffers from historical amnesia and revisionism” (p. 139). (This is silly and very uninformed for someone who talks the discourse of bioethics. See: Dominic Sisti’s work on new asylums).
On the topic of deinstitutionalization, Jeffreys writes:
“A final point I want to make regarding mental health care concerns[,] mass incarceration and mental hospitals. Contemporary criminologists and historians debate why the U.S. penal population has ballooned so incredibly in the past few decades. They offer competing explanations (the New Jim Crow, the power of prosecutors, the war on drugs, the rise of victims’ advocacy groups, economic interests), all of which illuminate this shocking phenomenon. However, only a few scholars (like Bernard Harcourt and Liat Ben-Moshe) have examined mass incarceration in light of the long U.S. tendency to incarcerate marginalized people. As I noted in chapter 2, Harcourt describes the extraordinary figure of 559,000 people in state mental hospitals in 1955. If we add to this figure other coercive (juvenile facilities, forestry camps, etc.), we have an extraordinary level of coercion in the United States even before the advent of mass incarceration. As Harcourt states, “simply put, when the data on mental hospitalization rates are combined with the data on prison rates for the years 1928 through 2000, the incarceration revolution of the late twentieth century barely reaches the level of aggregated institutionalization that the United States experienced at midcentury” (Harcourt 2006, 1754). When thinking about jails and mental illness, we should locate this phenomenon in the United States’ long and ugly history of incarcerating marginalized people. Only if we honestly confront this history will we be able to avoid simplistic responses to our current crisis of mental health care” (pp. 139-140; emphasis added).
Graph from 2006 article by Bernard Harcourt: “From the Asylum to the Prison: Rethinking the Incarceration Revolution.”
This is kinda an absurd comparison. Absurd comparisons can be useful, of course, when treated with care. But this needs some untangling. What Jeffreys is implying here is that we’ve simply moved the mentally ill out of hospitals and into prisons. But the data is NOT saying that. The prison rate ISN’T “mentally ill in prison.” It’s just total prison population, mentally ill or not mentally ill. Also, hospital and prison populations were very different: hospital patients were older, whiter, more female. Not just moving the same population. The graph – Jeffreys’s interpretation of it anyway – seems to imply that we just emptied the hospitals into the prisons. What really happened is far more complex and harder to disentangle. Obviously attitudes about treating various populations has changed during the 1970s. I am NOT saying that the lines aren’t causally linked. But the link is far more complex than a simple one-line-down-up graph suggests. Sadly, the last rigorous analysis of mental health problems among inmates was conducted in 2006 by the Department of Justice (DOJ) – more than a decade ago. Finally, there is another stats challenge with the prison-vs-civilian mental health comparisons: all people are screened for mental illness upon entering jails and prisons so we can imagine that this will lead us to overestimate the frequency of mental illness problems in prison vs. outside of prison: census vs. imperfect sample. That’s not saying “it’s not a big deal.” If anything, it likely signals how much undiagnosed mental illness exists outside prison. And to be clear, we seriously mistreat the mentally ill who are incarcerated and we always overlook the mental health harms of prison. But that doesn’t change the fact that Jeffreys’s interpretation in this quote tells a far too simplistic story about mass incarceration and mental health. (Not to mention that he seems to be suggesting that New Jim Crow, the power of prosecutors, the war on drugs, the rise of victims’ advocacy groups, economic interests are all simplistic stories which is bonkers).
(FYI: The best work I’ve seen on deinstitutionalization and prisons (not jails) suggest about a 4% to 7% prison growth from deinstitutionalization — see: Raphael & Stoll (2013) “Assessing the Contribution of the Deinstitutionalization of the Mentally Ill to Growth in the U.S. Incarceration Rate”).
References
Ben-Moshe, Liat, Chris Chapman, and Allison C. Carey (Eds). 2014. Disability Incarcerated: Imprisonment and Disability in the United States and Canada. New York: Palgrave Macmillian.
Brown, Michelle. 2009. The Culture of Punishment: Prison, Society, and Spectacle. New York: New York University Press.
Brown, Michelle. 2014. Visual Criminology and Carceral Studies: Counter-Images in the Carceral Age. Theoretical Criminology 18 (2): PAGES.
Geltzer, Jeremy. 2018. “Fake News & Film: How Alternative Facts Influence the National Discourse.” Southwestern Law Review 47: 297–334.
Gornick, Vivian. 1993. “The Reliable Reporter and the Untrustworthy Narrator.” Soundings 76 (2-3): 267–80.
Harris, Joseph. 2006. Rewriting: How to Do Things with Texts. Logan, Utah: Utah State University Press.
Nussbaum, Martha C. 2004. “Danger to Human Dignity: The Revival of Disgust and Shame in the Law.” The Chronicle of Higher Education 50 (48): B6.
Metzl, Jonathan M. and Kenneth T. MacLeish. “Mental Illness, Mass Shootings, and the Politics of American Firearms.” American Journal of Public Health 105 (2): 240–9.
Mogul, Joey L., Andrea J. Ritchie, and Kay Whitlock. 2011. Queer (In)Justice: The Criminalization of LGBT People in the United States. Boston: Beacon Press.
Ross, Jeffrey Ian. 2015. “Varieties of Prison Voyeurism: An Analytic/Interpretive Framework.” The Prison Journal 95 (3): 397–417. Available at SSRN: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2685252.
Smart Pills for Psychosis
The Tricky Ethical Challenges of Digital Medicine for Serious Mental Illness
I recently published a commentary on Abilify MyCite, the first smart drug approved for the treatment of schizophrenia and bipolar disorder in the American Journal of Bioethics.
I wrote about my lived experience with schizophrenia, neuroethics, and the importance of first-person accounts of illness in research and practice in: “The Missing Subject in Schizophrenia” — for the The Neuroethics Blog @ Emory University.
Carel, Havi. Phenomenology of Illness. New York: Oxford University Press, 2016.
My review of this book is on Metapsychology Online Reviews.